This Dr. Axe content is medically reviewed or fact checked to ensure factually accurate information.
With strict editorial sourcing guidelines, we only link to academic research institutions, reputable media sites and, when research is available, medically peer-reviewed studies. Note that the numbers in parentheses (1, 2, etc.) are clickable links to these studies.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
This article is based on scientific evidence, written by experts and fact checked by our trained editorial staff. Note that the numbers in parentheses (1, 2, etc.) are clickable links to medically peer-reviewed studies.
Our team includes licensed nutritionists and dietitians, certified health education specialists, as well as certified strength and conditioning specialists, personal trainers and corrective exercise specialists. Our team aims to be not only thorough with its research, but also objective and unbiased.
The information in our articles is NOT intended to replace a one-on-one relationship with a qualified health care professional and is not intended as medical advice.
Rheumatoid Arthritis Symptoms and 5 Natural Treatments
June 17, 2016

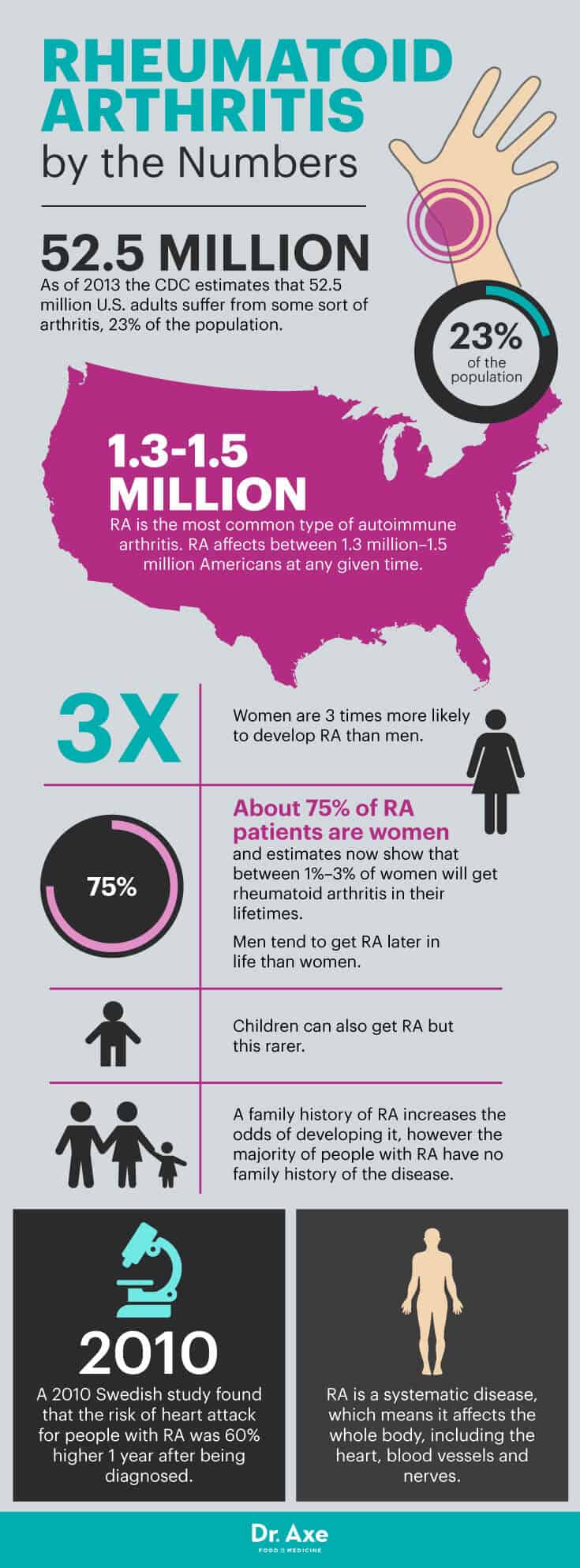
As I’m sure you’re well aware, an estimated 52.5 million U.S. adults suffer from some sort of arthritis, and one common form is rheumatoid arthritis (RA). (1) How wide does this disease cast its net? Rhematoid arthritis affects a staggering 1.3 million to 1.5 million Americans at any given time.
Thus the question arises: Is there anything you can do about this? As a matter of fact, there are a few things you can do to treat rheumatoid arthritis symptoms, and it starts with, well, knowing what those common rheumatoid arthritis symptoms are.
Let’s take a look at what RA is, the most common RA symptoms, and all-natural treatments for this form of arthritis.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disease that affects someone’s joints and causes ongoing pain, swelling, stiffness and limitations in terms of movements. For most people, their rheumatoid arthritis symptoms tend to flare up at times and become worse when inflammation levels rise, but then become better for a while, only to return once again. Currently, there is no “cure” for RA, only ways to manage rheumatoid arthritis symptoms and inflammation. When RA isn’t managed well, complications can develop over time, including significant joint damage, hormonal changes, nerve damage and dangerous inflammation of blood vessels.
While many adults experience some form of pain and inflammation at one time or another, RA is different because it tends to last for years and usually affects joints on both sides of the body simultaneously (for example, if one hand persistently hurts, a sign of RA is that the other one does too). The underlying cause of RA is inflammation, which is triggered by autoimmune reactions and causes joints to deteriorate over time.
Like with other autoimmune disorders, RA is caused by a combination of factors related to genetics, someone’s environment and lifestyle (including diet and level of activity), and someone’s hormones and immune system. When someone has arthritis, a person’s immune system attacks his or her own healthy body tissue and causes loss of cartilage. Because high levels of inflammation are lurking below the surface whenever someone has rheumatoid arthritis, RA commonly affects other parts of the body, including vital organs and the endocrine glands.
Studies show that people who receive early treatment for arthritis feel better sooner, have better quality of lives long term, and reduce the need or surgeries or risk for complications. (2) While medications are commonly prescribed to people with RA, holistic experts today recommend that RA patients take an involved “self-care” approach to managing their rheumatoid arthritis symptoms, including improving their diets, staying active and reducing pain naturally. Being proactive about reducing inflammation and other risk factors associated with RA can help improve someone’s quality of life and doesn’t pose the risk for side effects that often come along with long-term medication use.
Rheumatoid Arthritis Symptoms and Signs
Rheumatoid arthritis symptoms are caused by the loss of cartilage in joints, inflamed tissue surrounding joints and a tightening gap between joints due to swelling. (3) With RA, synovial fluid that normally lubricates joints starts to thicken and swell, while at the same time cartilage loss causes increased friction between joints and bones. The result is that joints become unable to move smoothly — weak, stiff, loose or unstable — and the buffering space normally between bones can become smaller, which limits range of motion.
- Joint pain — Swelling in and around certain joints lasts for six weeks or more. Any joint can become damaged due to RA, but the wrists, feet, hands, ankles and knees are most commonly affected.
- Redness, heat and tenderness near inflamed joints — Pain and tenderness are usually experienced in a “symmetrical pattern,” meaning multiple joints are impacted and on both sides of the body instead of just one (which can indicate an injury such as tendonitis or even osteoarthritis).
- “Morning stiffness” that’s usually worse right after getting up and lasts for 30 minutes or more — Some people experience morning stiffness for several hours just about every morning.
- Fatigue and muscle aches
- Trouble moving normally, including bending over, climbing stairs, walking or exercising
- For some people a loss of appetite or low-grade fever
What are some of the ways that you can tell if a flare-up in rheumatoid arthritis symptoms is coming up? Intense morning stiffness, redness and fluid retention are all good clues. Flares can sometimes mimic fevers or infections and cause feelings of general “crumminess.” Although arthritis flare-ups are somewhat unpredictable, for many people they’re most likely to hit after a very stressful situation, since emotional or physical stress is a “trigger” for many people that wears down the immune system. (4)
Arthritis Complications
For some people, RA causes long-term complications due to increased inflammation throughout the body. This is known as “systematic arthritis” or sometimes “inflammatory arthritis.” (5) Studies have found that complications of rheumatoid arthritis can include:
- Higher risk of heart disease and stroke
- Shortness of breath, chest pains, and trouble breathing normally due to lung scarring and damage
- Heart problems and nerve damage, caused by decreased circulation and inflammation of blood vessels (called vasculitis)
- Carpal tunnel syndrome
- Frequent headaches
- Kidney problems and fluid retention
- Bone pain and bone thinning
- Anemia and fatigue
- Enlarged spleen and low blood cell count
- Small lumps of tissue that develop around swollen joints below the skin — These are called “rheumatoid nodules” and can add to redness or pain. About half of people with RA get rheumatoid nodules, which are most common in bony areas exposed to frequent movement/pressure (like the fingers or elbows)
- Skin rashes, redness, heat, bruising and ulcers near the nail beds
- Impaired vision and eye problems, such as photosensitivity, dryness, redness and pain known as Sjögren’s syndrome
- Frequent infections in the mouth and gums
- Appetite changes, weight gain or weight loss

What Causes Rheumatoid Arthritis?
RA is an autoimmune disease, which means it’s triggered due to faulty reactions of the immune system that cause certain cells/chemicals to mistakenly attack the body’s own healthy tissue. The type of inflammation that causes RA is that which develops in the “synovium,” the tissue that lines the joint. The immune system’s destructive chemicals wear down cartilage that normally cushions the space between joints and bones, causing friction and pain.
Why would the immune system attack the body and create inflammation in tissues, including the joints? Inflammation associated with RA can be triggered by a number of factors, and risk factors include: (6)
- Poor gut health or “leaky gut syndrome“
- A poor diet and food allergies (foods that contribute to inflammation include refined carbohydrates, fried foods and too much sugar) (7)
- Obesity (especially if someone was obese before the age of 55)
- Genetic factors (certain genes can affect the immune system may make some people more prone to getting autoimmune disorders)
- Toxicity, due to things like environmental toxin exposure and endocrine disruptors
- Low immune function due to other medical conditions or autoimmune disorders
- Smoking cigarettes
According to the American College of Rheumatology, RA can sometimes be hard to properly diagnose and differentiate from other autoimmune diseases (like lupus or fibromyalgia) because their symptoms can all be similar at times. There isn’t one test that’s used to diagnose RA — rather a rheumatologist (a doctor who specialize in diseases that affect joints, bones and muscles) makes a diagnosis by evaluating a patient’s symptoms, medical history, family history and lifestyle. Taking a complete medical history, having a physical exam performed, and sometimes getting X-rays or a blood test can all help a doctor make a diagnosis.
Rheumatoid Arthritis vs. Lupus vs. Osteoarthritis
Lupus is another autoimmune disorder that’s systematic in nature and can cause similar symptoms to rheumatoid arthritis. Like with RA, lupus can affect the nerves, blood vessels, heart, kidneys, liver and endocrine system. Symptoms of lupus are frequently mistaken for other health problems or autoimmune disorders since they also occur in flare-ups and can include achiness, fatigue, swelling, joint pain, rashes and fever.
A few differences exist between lupus and RA. One is that lupus very commonly causes a hallmark “butterfly rash” on the face and usually also noticeable fatigue. To help differentiate the two and make proper diagnoses, doctors use a combination of tests, including antibody blood tests, c-reactive protein tests, urine tests, medical examination and family history. (8)
The Lupus Foundation of America points out that it’s also possible for someone with lupus to have rheumatoid arthritis (or another condition) and lupus at the same time. Doctors call this “overlap.” An overlap diagnosis is made when a patient meets the official criteria for two autoimmune diseases, and if this is the case it can be hard to tell which disorder causes symptoms on any given day. (9)
How can you tell the difference between RA (autoimmune arthritis) and osteoarthritis (non-autoimmune arthritis)?
Many people suspect they have RA when they experience morning stiffness and other symptoms associated with an autoimmune disorder. Usually osteoarthritis does not cause prolonged morning stiffness or symptoms like low-grade fever, fatigue, appetite changes and more frequent infections. Osteoarthritis is not an autoimmune disorder so it’s not caused by the immune system mistakenly attacking the body’s tissues. The causes of osteoarthritis are mostly inflammation, overuse of joints, or wear-and-tear damage associated with aging. Osteoarthritis does not usually affect the lining of joints or cause bone erosion and joint deformity because it’s not autoimmune in nature — it’s a degenerative joint disease instead.
The good news about these related health conditions is that over the past several decades the outlook has greatly improved for many people with newly diagnosed arthritis or autoimmune disorders. The same natural treatments for RA that you’ll learn about below can also help treat lupus or manage symptoms from other disorders by targeting underlying inflammation and improving immune functions.
RA Facts and Prevalence
- As of 2013, the Centers for Disease Control and Prevention estimate that 52.5 million U.S. adults suffer from some sort of arthritis — equating about 23 percent of the population.
- Rheumatoid arthritis is the most common type of autoimmune arthritis. RA affects between 1.3 million and 1.5 million Americans at any given time.
- Women are three times more likely to develop RA than men. (10) About 75 percent of RA patients are women and estimates now show that between 1 percent to 3 percent of women will get rheumatoid arthritis in their lifetimes.
- RA often starts in middle age, usually between the ages of about 30–60, and is most common in older adults (children can also get RA but this rarer). Men tend to get RA later in life than women.
- A family history of RA increases the odds of developing it, however the majority of people with RA have no family history of the disease.
- RA is a systematic disease, which means it affects the whole body, including the heart, blood vessels and nerves. A 2010 Swedish study found that the risk of heart attack for people with RA was 60 percent higher one year after being diagnosed.
Natural Treatment for Rheumatoid Arthritis Symptoms
Doctors practicing conventional medicine commonly use a combination of prescription drugs — like anti-inflammatories, corticosteroids, biologic agents that alter the immune system or painkillers — to help control RA symptoms. While these are necessary for some people, natural treatments can also make a huge impact in terms of helping lower pain, reduce swelling, prevent further joint damage and increase someone’s quality of life. Natural treatments also won’t cause unwanted side effects, which are common due to arthritis medication use — including liver damage, anemia, low platelet count, hair loss, kidney issues and heart problems. (11)
Here are some ways you can manage rheumatoid arthritis symptoms and prevent complications from developing naturally:
1. Eat an Anti-inflammatory Diet
High-antioxidant foods and those that are “whole”/unprocessed help control RA symptoms best. Experts emphasize the importance of eating a healthy “arthritis diet” that includes healthy fats like olive oil and coconut oil, plenty of fresh vegetables and fruits, bone broth, high-sulfur foods and foods naturally high in omega-3s (like wild-caught fish and nuts/seeds). In fact, a 2018 human study revealed that rheumatoid arthritis (RA) patients who consumed fish more than twice a week experienced lower RA activity. For each additional serving of fish, patients reported even lower RA activity levels. (12) It’s also important to steer clear of foods that trigger inflammation — like added sugar, synthetic ingredients, hydrogenated/trans fats, fast foods and common allergens like gluten or pasteurized dairy.
2. Stay Active
Although RA can cause flare-ups of pain along with limited range of motion, staying active in general is a very important for controlling symptoms and managing joint inflammation. Joint pain associated with RA tends to be worse after periods of inactivity (which is why sleeping causes morning stiffness) so exercise has many benefits. (13)
The best type of activities or exercises for people with rheumatoid arthritis are those that are low-impact and don’t overly stress sensitive joints, including cycling, walking, water aerobics and yoga. Your exercise routine should ideally combine a form of aerobic activity with strength training and stretching to improve flexibility, muscle strength and cardiovascular health. When symptoms become very bad, extra rest is helpful — however, stretching can still help manage inflammation.
3. Manage Stress and Get Enough Sleep
Getting enough sleep and limiting emotional stress allow joints to heal best, so these habits are especially important during episodes of increased inflammation, pain, swelling and stiffness. Fatigue and stressful episodes tend to make inflammation worse and can also contribute to complications like muscle pains, low immunity, infections, overeating, inactivity and weight gain.
Studies have found that by practicing relaxation techniques — such as guided meditation, yoga or stretching, deep breathing, guided imagery, and visualization — you have better protection against painful episodes since these help your muscles relax, balance hormones, decrease cortisol and strengthen your immune system. In fact, the Arthritis Foundation points out that stress-relieving activities, having a positive attitude and receiving support from family/friends have been shown to significantly help patients with RA cope with their pain. (14)
4. Control Pain Naturally
Research shows that natural pain-reducing techniques, including massage therapy, acupuncture or acupressure, essential oils used on the skin, and heat/ice treatments (like ice packs or warm baths) all help manage rheumatoid arthritis symptoms. Many of these can double as natural stress relievers since they improve body awareness, help you stay active, can help with sleep, and ease stress or anxiety. Essential oils for arthritis include ginger, orange, myrrh, frankincense and turmeric oils. You can also try using topical treatments on the skin containing salicylates or capsaicin, which some studies show help reduce joint pain. (15)
5. Reduce Inflammation with Supplements
Anti-inflammatory supplements that can help reduce arthritis pain include:
- turmeric and ginger extract
- boswellia/frankincense
- omega-3 fish oils
- proteolytic enzymes
- glucosamine
- MSM
Final Thoughts on Rheumatoid Arthritis Symptoms
- An estimated 52.5 million U.S. adults suffer from some sort of arthritis — or 23 percent of the adult population — and there is no more common form than rheumatoid arthritis. Rheumatoid arthritis symptoms affect 1.3 million to 1.5 million Americans at any given time.
- RA tends to last for years and usually affects joints on both sides of the body simultaneously.
- The most common rheumatoid arthritis symptoms include joint pain; redness, heat and tenderness near inflamed joints; morning stiffness; fatigue and muscle aches; trouble moving normally; loss of appetite; and low-grade fever.
- Inflammation associated with RA can be triggered by a number of factors, including poor gut health or leaky gut syndrome, a poor diet and food allergies, obesity, genetics, toxicity, low immune function, and smoking.
- Women are three times more likely to develop RA than men. About 75 percent of RA patients are women and estimates now show that between 1 percent to 3 percent of women will get rheumatoid arthritis in their lifetimes.
- You can naturally treat rheumatoid arthritis symptoms by eating anti-inflammatory foods, staying active, managing stress and getting enough sleep, controlling pain naturally, and reducing inflammation.
