Men at high risk of developing prostate cancer would benefit from a change in NHS prostate cancer guidelines, experts say.
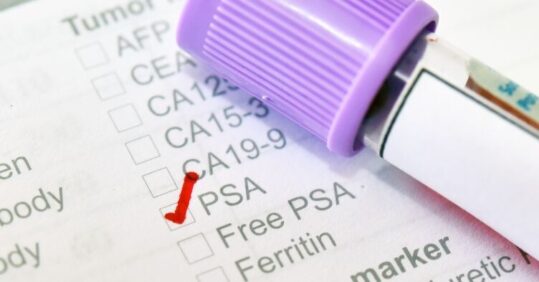
Researchers suggest that NHS prostate cancer guidelines should allow GPs to proactively discuss prostate-specific antigen (PSA) tests with people who are at high risk of developing the disease.
In a paper published in the British Journal of General Practice, urology and prostate cancer experts from the University of Manchester, Prostate Cancer UK, and other institutions say there is strong evidence that changing the guidelines could save lives and ‘smash inequalities’.
Black men and men with a family history of the disease are at the highest risk of developing the disease and tend to develop cancer at a younger age, but under current NHS guidelines, these men are not told about their chance of getting the disease. The change to the guidelines would allow healthcare professionals to talk to men from the age of 45 who are considered high-risk.
The researchers said this type of proactive healthcare could also help deliver one of the Government’s manifesto pledges to save lives through earlier diagnoses and tackle racial and regional health inequalities.
Current NHS guidelines do not recommend screening for prostate cancer in the UK. Asymptomatic men under the age of 50 can request a PSA test if counselling is also undertaken; however, levels of clinical uncertainty among GPs result in varying quality of care. The report aimed to produce a consensus that can influence guidelines for UK primary care on the best use of the PSA test for early prostate cancer detection in asymptomatic men.
In the earliest stages of prostate cancer, there are often no symptoms, and the experts argue that it is crucial that men know their risk of getting and are offered the option of getting a PSA blood test. Current data shows only half (53 per cent) of men with prostate cancer get an earlier diagnosis, which is significantly below the NHS’s target of 75 per cent. Black men have double the risk of both getting prostate cancer and dying from the disease, while men living in deprived areas of the UK are 29 per cent more likely to be diagnosed with incurable disease.
Dr Sam Merriel, a GP and academic clinical lecturer at The University of Manchester and one of the authors of the paper, said: ‘As a GP, it’s frustrating that current Department of Health and Social Care guidelines on PSA testing in men without symptoms provide very limited detail for us and our patients. It is unclear what should be done for men at higher risk of prostate cancer, how often men who choose to have the PSA blood test should have one, and when it would be in a man’s best interest to stop testing.’
In the PSA Consensus paper, the researchers state that the PSA blood test is a cheap, safe, and effective way of identifying which men would benefit from further tests, such as an MRI. Prostate Cancer UK estimates that updating the NHS guidance and implementing the plans for raising awareness about the changes could be delivered in just 12 months.
Dr Merriel said there were ‘disagreements’ about the benefits and harms of the PSA blood test but added: ‘With the publication of this new paper, we’ve shown there’s broad agreement among the top minds in urology and prostate cancer care that the PSA blood test is simple and safe – and that GPs should consider proactively discussing the test with Black men and men with a family history from the age of 45.’
The researchers acknowledge that increases in PSA testing are likely to pose a ‘substantial challenge’ to already overstretched primary care resources and suggest that the Government will need to provide the extra resources.
Amy Rylance, assistant director of health improvement at Prostate Cancer UK, added: ‘Leaving men in the dark about their risk means too many men are getting diagnosed with incurable prostate cancer, and this disproportionately affects Black men and men living in deprived areas. Updating NHS prostate cancer guidelines could drive forward significant progress in just a year and, crucially, would give men a fairer chance of living longer.’