At the Royal Victoria Hospital in Belfast, patients waiting for heart surgery attend a pre-operative education session. This initiative won the Surgical Nursing category in the 2017 Nursing Times Awards
Abstract
Waiting for a heart operation is often a stressful time for patients and their families, during which they have little contact with, and receive little support from, the hospital team. The Royal Victoria Hospital in Belfast introduced pre-surgery education sessions for patients and relatives. It is too early to establish whether this will have long-term health benefits for patients, but already waiting times have dropped dramatically and patients are better prepared for surgery, mentally and physically.
Citation: Cassidy A (2018) Educating and supporting patients awaiting elective cardiac surgery. Nursing Times [online]; 114: 8, 42-43.
Author: Aileen Cassidy is clinical coordinator in cardiothoracic surgery at the Royal Victoria Hospital, Belfast Health and Social Care Trust.
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
- To contact Aileen Cassidy about this project, please email: aileen.cassidy@belfasttrust.hscni.net
Introduction
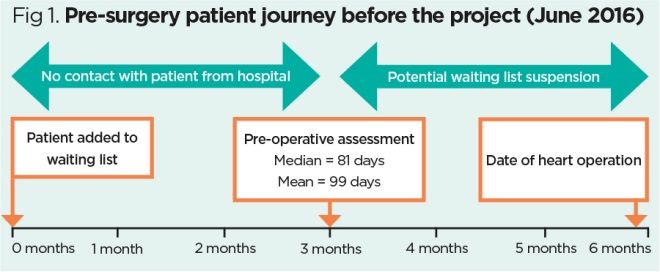
In Northern Ireland, patients wait six months or more for elective cardiac surgery. After joining the waiting list, the next time they meet someone from the healthcare team is at their pre-operative assessment, some three or four months later. This waiting time could be used to optimise their health but the opportunity is usually missed and, instead, many patients experience stress, anxiety and isolation.
To address these concerns, in January 2016 the cardiac surgery pre-assessment team, patient schedulers and management at the Royal Victoria Hospital in Belfast carried out a process-mapping exercise of the cardiac surgery patient’s journey. One recommendation to emerge was that an education programme should be created for these patients and their families so, in June 2016, the pre-assessment team and patient schedulers began devising a programme to:
- Encourage patients to optimise and take responsibility for their health before surgery;
- Address patients’ and relatives’ stress and other psychological problems;
- Shorten waiting times for pre-operative assessment appointments and surgery, thereby improving access;
- Reduce waiting list suspensions and last-minute cancellations.
Conditions and comorbidities
Most of our patients have life-threatening conditions such as: coronary artery disease; aortic, mitral or tricuspid valve disease; thoracic aortic aneurysms; and congenital heart defects. They require major open-heart surgery such as coronary artery bypass grafting, heart valve surgery and replacement of the aorta. Ranging in age from teenagers to octogenarians, they often have comorbidities.
Many patients experience severe symptoms that significantly reduce their ability to perform activities of daily living, forcing them to change their lifestyles and rely on help from others. They often live in fear of having a heart attack or of their health deteriorating further while awaiting surgery. Before we introduced the education programme, when our patients finally attended their pre-assessment appointment, they often reported having felt isolated, ‘like a ticking time bomb’ or ‘like a number’.
Education programme
Patients are invited to attend an education session two to three weeks after joining the waiting list. We encourage them to come with a relative or friend, as support from people close to them is key in helping them. Each session, which lasts two to three hours and takes place every two to three weeks, is attended by up to 15 patients and their relatives, and delivered by myself and/or a pre-assessment nurse.
During the session, we discuss the patient journey while they are waiting for surgery and what they can expect during their hospital stay and after discharge. We advise them how to manage their symptoms and stay safe while awaiting surgery, and encourage them to start improving their health. This includes – where appropriate – advice on diabetes control, smoking cessation, weight management, reducing alcohol consumption and dental care. We explain cardiac rehabilitation and what patients may need to do after surgery to ensure they recover fully. Patients have the opportunity to ask questions and speak to other people in similar situations.
The education programme has brought changes to other aspects of the pre-surgery journey. When attending their pre-operative assessment appointment, patients have already received extensive information so more time can be spent addressing specific aspects of their condition. Issues that might delay surgery can also be identified, and investigations ordered.
Venue
The first education session was held in a meeting room in the hospital grounds, but patients had problems parking and the venue was quite far from the car park, which created difficulties for those with effort-induced symptoms such as angina. We therefore found a local venue 1.2 miles from the hospital, with free parking, helpful staff and conference rooms. Each session is now held there at a cost of approximately £120 (including tea and scones).
An additional benefit of the venue is that patients can stay there the night before surgery if they live far away. This is organised and funded by the hospital, including accommodation for next of kin if needed. Patients are already familiar with the location and know how to get there, which reduces stress just before surgery.
Patient feedback
We were concerned that patients might feel the education session was “one visit too many” to Belfast in relation to their surgery. However, the feedback via questionnaires shows that they and their relatives derived great benefit from the session. In formal feedback collected via a patient experience collaborative, patients spoke of their positive experience of the programme and how well it prepared them for surgery.
“Empowering patients and relatives at a very stressful time, this project dramatically improved the patient pathway and patient safety” (Judges’ feedback)
Informal feedback from conversations with patients after surgery has also been extremely positive. They appreciated the physical and psychological preparation, shorter waiting time and improved access. They said they felt reassured, supported and empowered. Some relatives who had had cardiac surgery in the past said they wished a similar programme had been available for them.
Team’s experience
Initially, there were some concerns among team members about workload and the fact that they would have to speak in front of large groups. However, everyone involved in delivering the session enjoyed it and derived great personal satisfaction from making a difference to patients’ lives.
One difficulty was getting the timing right, both in terms of session frequency and length, but this was addressed through team work, meetings, reviewing processes and open communication. As a result, the booking process has become more routine, resulting in a smoother patient experience.
Outcomes and next steps
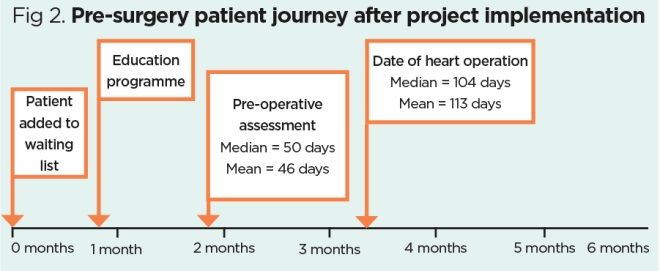
We do not yet know how effective the education programme will be in improving patients’ health in the long term; however, we have seen a reduction in the number of patients suspended from the waiting list because of lifestyle factors such as poor diabetes control, overweight or failure to stop smoking. There has also been a dramatic reduction in waiting times: patients now wait just over three months for surgery, as opposed to almost six months. They also attend their pre-assessment appointment much earlier. Figs 1 and 2 show the patient journey before and after the introduction of the programme.
Our plans for the future include recruiting a patient representative to help us improve the programme further. We also intend to audit it more rigorously so we can provide reliable data on metrics such as patient outcomes, waiting times and access to services.
Key points
- The waiting time before cardiac surgery can be put to good use to optimise patients’ health
- Patients awaiting cardiac surgery often experience stress and anxiety
- Health improvement advice for patients awaiting cardiac surgery should cover diabetes, smoking, weight, alcohol use and dental care
- A pre-surgery education programme at a hospital in Belfast has received positive feedback from patients
- Since the programme was created, waiting times and the number of suspensions from the waiting list have decreased

Have your say
or a new account to join the discussion.