Nuffield Health trains hospital matrons to be effective leaders in infection prevention and control. This initiative won the Infection Prevention and Control category in the 2017 Nursing Times Awards
Abstract
The role of director of infection prevention and control was introduced in the UK in 2003 to ensure effective leadership in infection prevention and control. In Nuffield Health’s 31 hospitals in the UK, the role is held by the hospital matron, who is the clinical lead (equivalent to a director of nursing in the NHS). However, matrons may not always have the knowledge and skills to be effective leaders in this area, and there was no director of infection prevention and control training in the UK. We identified that our matrons had gaps in their knowledge and in 2014 launched our own education programme to help improve reporting and reduce infection rates.
Citation: Millward S (2018) Enhancing leadership in infection prevention through training. Nursing Times [online]; 114: 9, 32-33.
Author: Sue Millward is quality lead infection prevention for Nuffield Health.
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
- To contact Sue Millward about this project, please email: Sue.Millward@nuffieldhealth.com
Introduction
In 2003, the chief medical officer’s report Winning Ways (Department of Health, 2003) stressed the need for effective leadership in infection prevention and control (IPC). There were concerns the NHS was not performing as well as health systems in other European countries regarding IPC and that hospitals in England were not consistently using evidence-based practice.
The role of director of infection prevention and control (DIPC), introduced in Winning Ways, was embedded in legislation in the DH’s Health and Social Care Act 2008: Code of Practice on the Prevention and Control of Infections and Related Guidance – known in the field of IPC as ‘the Code’; it was first published in 2010 and updated in 2015 (DH, 2015).
In the NHS, the DIPC role is usually held by a microbiologist, infection prevention nurse (IPN) or senior clinical lead. In the independent sector, DIPCs tend to be hospital matrons (equivalent to directors of nursing in the NHS) because they lead all hospital clinical staff including nurses, allied health professionals and the resident medical officer.
IPC leadership
Nuffield Health is an independent, not-for-profit healthcare organisation that runs 31 acute hospitals (1,600 beds in total) spread across the UK. A chief executive officer manages the organisation, supported by a chief nurse and a national IPN (known as the quality lead infection prevention). Each of the 31 hospitals is managed by a hospital director who holds the regulatory title of registered manager and has executive responsibility for IPC (as does a chief executive officer in an NHS trust).
The senior clinical lead in each Nuffield Health hospital is the matron, who also holds the DIPC role and is, therefore, accountable for infection prevention at a local level. The matron is a member of the senior management team and reports directly to the hospital director, deputising for them in their absence.
As DIPCs, our hospital matrons are responsible for implementing evidence-based practice, challenging poor practice and ensuring robust audit and surveillance processes so infection risks are promptly detected, reported and acted on, in line with DH (2015) guidance. They are supported by an IPN or an IPC coordinator – IPC coordinators being trained infection prevention link practitioners (IPLPs).
Knowledge gap
DIPCs must understand their responsibilities under the DH’s Code for IPC. Microbiologists and IPNs will normally have the right knowledge and skills to fulfil the role, but this is not necessarily the case of senior nurses holding director roles, such as hospital matrons. In 2014, following discussions with our matrons and a review of surveillance data and processes, we identified a gap in the knowledge and skills of matrons regarding healthcare-associated infections (HCAIs), standard IPC precautions and regulatory requirements for reporting infections. We also identified that there were no DIPC educational programmes in the UK. This led us to develop our own postgraduate DIPC educational programme.
Programme content
We designed a two-day programme that placed equal emphasis on theory and practice. To help us deliver it and ensure credibility and professional development, we approached De Montfort University in Leicester. The core content comprises:
- Microbiology and HCAIs;
- Regulatory requirements for IPC and antimicrobial stewardship;
- How to detect trends and risks through surveillance and audit;
- Standard IPC precautions, including hand-hygiene competency assessments.
We want participants to be able to:
- Understand the emergence of HCAIs and the implications for patients, visitors and the organisation;
- Evaluate the role of the DIPC in the multidisciplinary team;
- Analyse the effectiveness of existing policy and guidance;
- Identify areas for improvement.
Learning outcomes are assessed through a practice assessment module and a 2,500-word assignment, which asks participants to critically analyse the role of healthcare practitioners in the provision of IPC.
Running the programme
The DIPC programme was launched in April 2014. It gives DIPCs theoretical knowledge and practical training, and is an opportunity to network and reflect on their role undistracted by day-to-day work pressures. We offer it twice a year, which allows us to train new matrons. Thirty-six of the 39 matrons who have attended so far have successfully completed it. The three matrons who have not, who came from other independent healthcare providers, left their jobs before they could complete the assignment.
Delivering an educational programme for four or five participants could be a challenge, but we mitigate this by running it alongside an established IPLP training scheme. This has significant benefits, including IPLPs and matrons working together for practical sessions – for example, on hand hygiene and using protective clothing.
Outcomes to date
Evaluation shows improved participant knowledge on microbiology, regulatory requirements and DIPC responsibilities. Participants reported feeling empowered to manage IPC and described the programme as ‘educational’, ‘useful’ and ‘worthwhile’:
“Really enjoyed the challenge. Wonderful to be able to focus on infection prevention away from the hospital environment with all the distractions that it causes.”
“Amazing work and innovation to set up this course, truly useful and interesting. Refreshed lots of my buried knowledge and gained some further knowledge.”
Participating matrons have also reported a series of service improvements in their respective hospitals, including:
- Appointment of two full-time IPNs and resources secured to train another four;
- Additional time allocated to IPC activities;
- Increased emphasis on IPC at senior management meetings;
- Commitment from the DIPC to ‘walk the floor’ with IPNs to discuss infections and review infection data;
- Improved communication and engagement with microbiologists.
Infection data reporting has improved: in 2015-16, all 31 Nuffield Health hospitals met the deadlines for reporting HCAIs to Public Health England, against 25 in 2014-15.
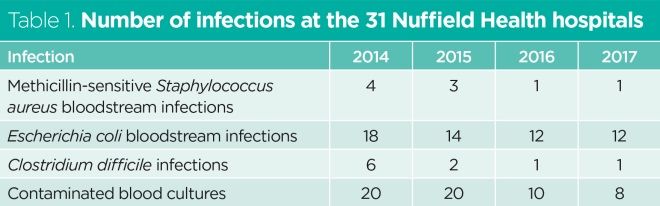
The programme is helping us to achieve lower infection rates: since 2014, we have seen a reduction in Clostridium difficile infections and methicillin-sensitive Staphylococcus aureus and Escherichia coli bloodstream infections in our hospitals (Table 1).
Conclusion
Developing an educational programme for DIPCs ensures our matrons are equipped for their role, surveillance and reporting are robust, and patient safety is enhanced through prompt detection of infection risk and appropriate action. Millward (2018) describes the programme and its achievements in more detail.
“The model is replicable and other organisations are already participating” (Judges’ feedback)
DIPCs at Nuffield Health are now engaged in IPC more than ever: attendance at a recent DIPC study day was excellent, with all 31 hospitals represented; external reporting is accurate and timely; staff participate in national and global campaigns, including the World Health Organization’s Clean Your Hands campaign on 5 May; DIPCs have update meetings twice a year; and infection prevention teams attend an annual infection prevention conference. This suggests our matrons are effective IPC leaders who help staff implement best practice to achieve lower infection rates and improve patient outcomes.
Key points
- Directors of infection prevention and control (DIPCs) were introduced in the UK in 2003 to ensure leadership in this challenging area
- The DIPC can be a microbiologist, an infection prevention nurse or a senior clinical nurse (director of nursing in the NHS or hospital matron in the independent sector)
- DIPCs may not always have the right knowledge and skills to fulfil the role
- A DIPC training programme can help ensure matrons provide effective leadership in infection prevention and control
- Nuffield Health has created a training programme to ensure its matrons are well equipped in their role as DIPC
Department of Health (2003) Winning Ways: Working Together to Reduce Healthcare Associated Infection in England.
Millward S (2018) Leading from the top: evaluation and impact of an educational programme for Directors of Infection Prevention and Control (DIPC) within the Independent Healthcare Sector (IS). Journal of Infection Prevention; e-pub ahead of print. DOI: 10.1177/1757177418786389.


Have your say
or a new account to join the discussion.