The fourth article in our series on respiratory rate is a guide to the assessment of breathing rhythm and chest movement, which provide important information on a patient’s condition
Abstract
Breathing rhythm and chest movement provide key information on a patient’s condition. The fourth article in this five-part series on respiratory rate expands on the procedure to measure respiratory rate outlined in part 3 and provides a guide to the assessment of respiratory rhythm and chest movement.
Citation: Wheatley I (2018) Respiratory rate 4: breathing rhythm and chest movement. Nursing Times; 114: 9, 49-50.
Author: Iain Wheatley is nurse consultant in acute and respiratory care, Frimley Health Foundation Trust.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
- Click here to see other articles in this series
Introduction
A changing respiratory rate (RR) measurement is cited as an early indicator of patient deterioration (Dougherty and Lister, 2015), but there are other respiratory signs that can be observed in conjunction with it.
In normal breathing a fairly steady rate, inspiratory volume and depth of chest movement are maintained, with equal expansion and symmetry. In the resting state normal breathing is relaxed, regulating the gas exchange in the lungs to maintain homoeostasis and balance pH changes and metabolism.
When there is an increased demand on the respiratory system from an acute episode, such as a chest infection, or long-term conditions, such as chronic obstructive pulmonary disease, the respiratory rhythm and chest movement change. These changes are compensatory mechanisms as a direct result of a chemical imbalance; and the primary cause may be mechanical, metabolic or neurological. The changes result in an increase or decrease in RR, depth of breathing and pattern of breathing.
Changes in rhythm and chest movements are made through feedback mechanisms to the central respiratory control centres of the brain. A range of receptors provide information that is interpreted in the higher respiratory centre, modulating RR and chest movement (Feldman and Del Negro, 2006); these receptors are:
- Peripheral chemoreceptors found in the carotid artery detect changes in PaO2 in the blood as well as PaCO2 and pH;
- Central chemoreceptors in the ventral medullary surface of the medulla oblongata in the brain detect pH changes;
- Mechanoreceptors are stretch receptors located in the smooth muscle of the main airways and parenchyma. They respond to excessive stretching of the lung during inspiration and send signals to the apneustic centre of the pons (located in the brain stem); the pons controls inspiration and expiration.
Respiratory rhythm and chest movement
Normal
In relaxed normal breathing the RR is 12-20 breaths per minute (bpm) (Royal College of Physicians, 2017). Chest expansion on inspiration should be the same or similar on each breath. The chest wall is symmetrical, accessory (neck and shoulder) muscles are not used, diaphragm muscles are functioning, and there is no paradoxical movement – the chest and abdomen move in the same direction on inspiration and expiration.
Abnormal
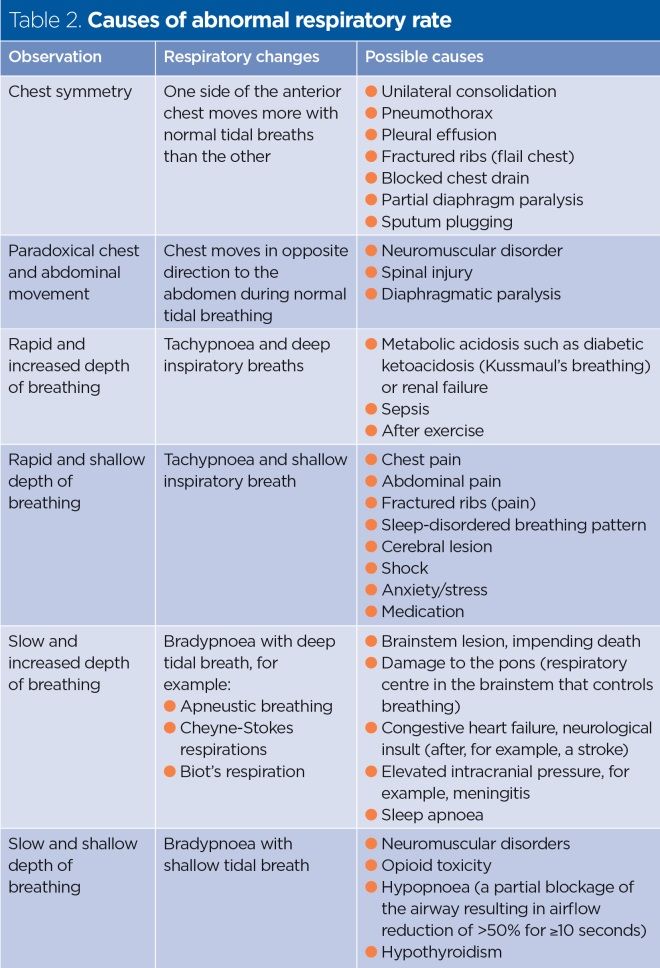
There are several reasons why respiratory rhythm and chest movement may change. Abnormality in respiratory rhythm may be related to changes in the patient’s metabolic state; for example, a patient with diabetic ketoacidosis may exhibit signs of rapid, deep breaths. Such breathing (often called Kussmaul’s breathing) aims to reduce the level of CO2 in the blood to maintain a normal pH and re-establish a homoeostatic state.
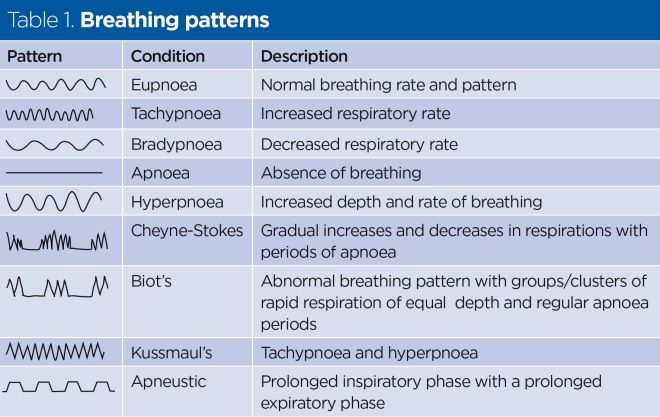
Patients with chest pain may have rapid but shallow breaths because deep breaths cause discomfort; in patients with rib fractures adequate pain relief is paramount to restore a normal depth and rate of breathing. Table 1 outlines common rhythm patterns, while Table 2 details key respiratory changes and possible causes.
The procedure
Observation of respiratory rhythm and chest movement can be incorporated into Wheatley’s (2018) procedure for assessing RR. The key principles of chest observation are outlined below. It is important to have a clear view of the chest so the chest area should be exposed. Protect the patient’s dignity at all times by screening the bed.
- Chest symmetry – standing in front of and facing the patient, observe whether the movement of both sides of the anterior chest is symmetrical.
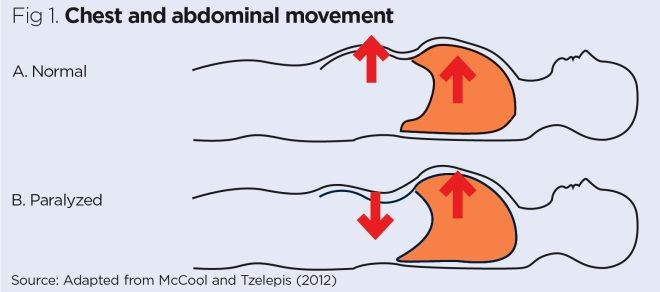
- Chest and abdominal movement – the chest and abdomen should move in the same direction during a normal tidal breath (Fig 1) but it can be difficult to observe this. Positioning the patient in a semi-recumbent position and observing the movement from the side gives the best view.
- Depth of chest movement – in normal tidal breathing the inspiratory and expiratory movement is fairly constant. Monitor for tachypnoea (>25bpm) or bradypnoea (<12bpm) and assess whether the tidal breath is very deep or shallow (RCP, 2017).
- Accessory muscle use – observe the patient from the front and note whether there is increased work of breathing at rest, which includes the use of the sternocleidomastoid (neck), scalene (shoulder), pectoral and abdominal muscles (Tulaimat and Trick, 2017). The patient may sit forward with their hands on their knees or resting on a table to relieve respiratory muscles and increase inspiratory capacity.
- Rhythm – breathing rhythm is usually constant and regular; a rhythm with abnormally long pauses between breaths or cessation of breaths and then rapid breathing is abnormal (Table 1).
Conclusion
It is important to observe RR and to examine the rhythm of breathing and movement of the chest when conducting a respiratory assessment. This observation can aid rapid diagnosis and treatment particularly in patients who are acutely ill.
Also in this series
Feldman JL, Del Negro CA (2006) Looking for inspiration: new perspectives on respiratory rhythm. Nature Reviews Neuroscience; 7: 3, 232-241.
McCool FD, Tzelepis GE (2012) Dysfunction of the diaphragm. New England Journal of Medicine; 366: 10, 932-942.
Royal College of Physicians (2017) National Early Warning Score (NEWS) 2.
Tulaimat A, Trick WE (2017) DiapHRaGM: a mnemonic to describe the work of breathing in patients with respiratory faialure. PLoS One; 12: 7: e0179641.
Wheatley I (2018) Respiratory rate 3: how to take an accurate measurement. Nursing Times; 114: 7, 21-22.

Have your say
or a new account to join the discussion.