1. INTRODUCTION
Annular pancreas is a rare congenital anomaly of the pancreatic ducts [1]. This anomaly is due to incomplete rotation of the ventral pancreatic bud. Annular pancreas is diagnosed with nearly equal frequency in children and adults [2]. The factors initiating symptoms are recurrent pancreatitis, duodenal stenosis, and duodenal or gastric ulceration [3].
One new case of duodenal obstruction due to annular pancreas is presented.
2. CASE REPORT
An 18-year-old man presented with a history of recurrent attacks of epigastric pain, nausea and vomiting. The symptoms had been present for more than 1 year, but had become more frequent in the last few months. On examination, he was found to have a Spanish sound. Side viewing duodenoscopy revealed an important concentric narrowing of the second part of the duodenum which could not be crossed. Computed tomography (CT) scanning showed an annular pancreas encircling the second part of the duodenum (figure 1).
Our patient was taken to laparotomy which confirmed the annular pancreas encircling the duodenum. The first part of the duodenum was dilated. This enlargement extended downward to the second part of the duodenum, which was markedly constricted by a ring of pancreatic tissue which completely surrounded the duodenum and which was continuous with the head of the pancreas. No

Figure 1. Computerized tomography of abdomen showing the annular pancreas encircling the second part of the duodenum.
other congenital anomaly of the intra abdominal organs was noted. A gastroenterostomy was performed without technical difficulty. The patient made an excellent recovery, and he was discharged from hospital 4 days later. He remains in good general health 6 months after the surgery (figures 2 and 3).
3. DISCUSSION
Annular pancreas was first described by Tiedman in 1818 [4], and named by Ecker in 1862 [5].
Only 737 cases of annular pancreas have been reported in the literature [1]. It is a rare congenital anomaly (the incidence is approximately 3 in 20000), and it is the most common anomaly of the pancreatic ducts after pancreas divisum [2].
Three developmental theories explain the formation of an annular pancreas. Baldwin in 1910 suggested that there was a failure of atrophy of the left component of the ventral pancreatic anlage which maintains a true ven-

Figure 2. Photograph of the annular pancreas.
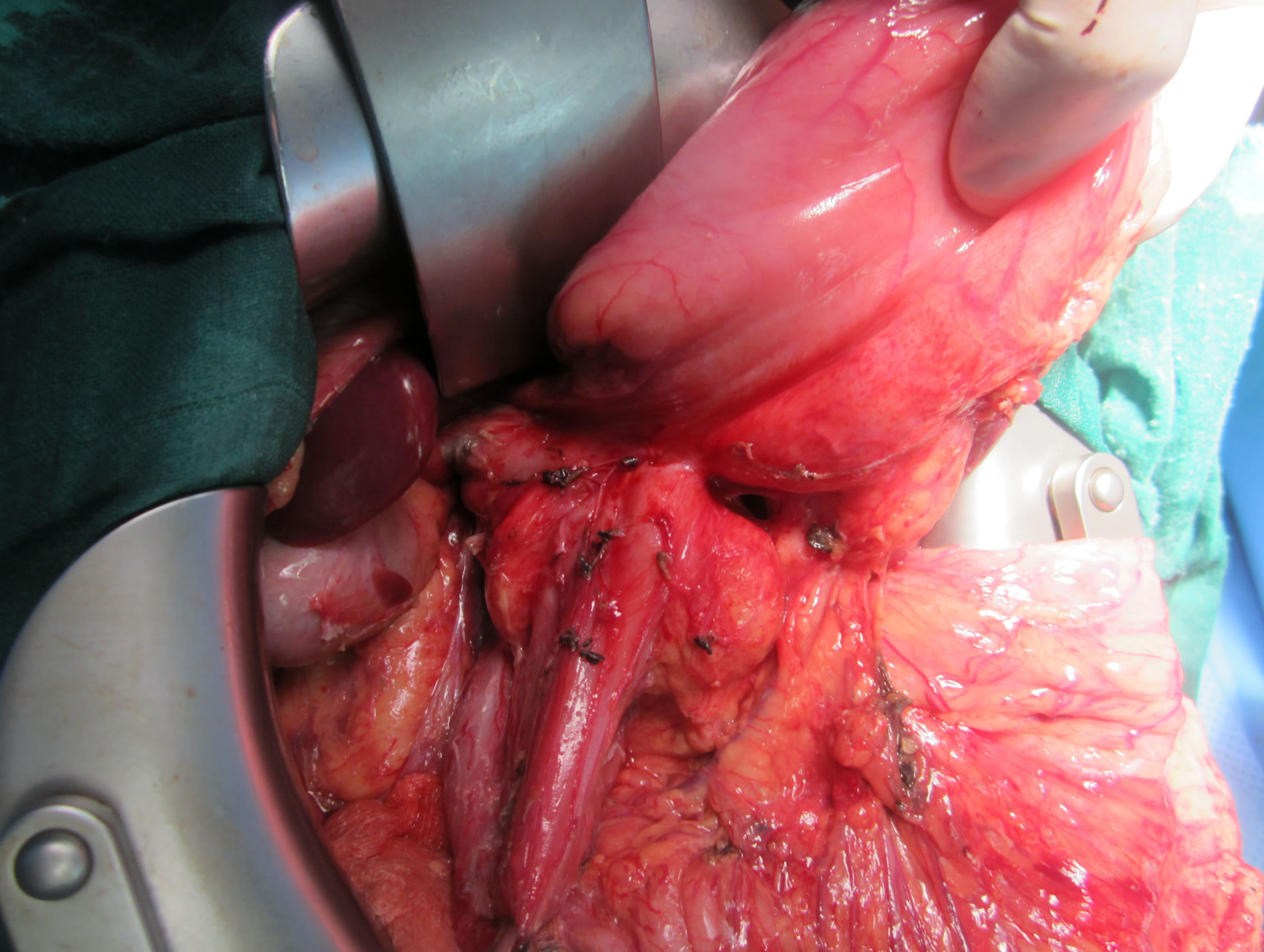
Figure 3. Intra-operative photograph showing an annular ring of pancreatic tissue around the duodenum.
tral connection [2]. Lecco’s theory suggests that the ventral pancreas adhered to surrounding tissues at its site of origin in the ventral mesogastrium maintaining a true ventral connection [6]. The third theory, explained by Verga in 1972 [7], suggests that the primary abnormality is duodenal with the pancreas “filling the space” around a narrowed duodenum. This results in a complete or incomplete stenosis of the duodenal lumen.
It has been estimated that only about 33% of the cases are symptomatic [3]. In children, annular pancreas appears most often in the first weeks of life by symptoms related to duodenal stenosis [2]; and other associated congenital malformations have been reported like common mesentery, heart defects, Down syndrome (Trisomy 21), imperforate anus, or tracheoesophageal malformations [2]. In adults, the age of revelation is usually between 20 and 50 years. The most frequently found symptoms are: abdominal pain (70%), vomiting and nausea (47%), and they are generally reflecting a proximal intestinal obstruction [8]. Other clinical manifestations have been reported: peptic ulcer secondary to stasis upstream of duodenal stenosis, acute or chronic pancreatitis due to the default flow of pancreatic secretions in the annular pancreas, and jaundice due to the common bile duct stenosis by the annular pancreas or related to a lithiasic origin [2,8].
The diagnosis of annular pancreas used to be based on duodenography which showed a medio duodenal stenosis corresponding to the pancreatic ring [8]. Nowadays, CT scan allows us to see the pancreatic ring encircling the duodenum [2]. The echo endoscopy also allows approaching the diagnosis by showing the ring of normal pancreatic tissue encircling the duodenum, but the pancreato MRI remains the most reliable diagnostic tool and allows to highlight the presence of a pancreatic duct encircling the duodenum [8,9]. Endoscopic retrograde cholangiopancreatography (ERCP) can also make the diagnosis, but it remains invasive and sometimes impossible in case of an uncrossable stenosis of the duodenal lumen [9].
The treatment of annular pancreas is surgical. Its aim is relief of the duodenal obstruction. For this, there are various procedures being used. The first one is to directly attack the obstruction by dividing or removing a portion of the annular pancreas despite the associated hazards of pancreatic or duodenal fistula [1,10]. Furthermore, the division of the annular pancreas is often followed by persistent symptoms, particularly abdominal pain (up to 50% of cases) [10]. On the other side, the majority of surgeons have elected to bypass the obstruction by establishing a gastrojejunostomy, a latero lateral anastomosis of the first part of the duodenum with the jejunum, or a duodeno-jejunal anastomosis with Roux en Y loop [3,10]. The frequent association of peptic ulcer and the risk of anastomotic ulcer suggest the need for a procedure like vagotomy which reduces acid secretion by the stomach. Thus from available evidence it appears corrective operations for annular pancreas should include vagotomy and gastrojejunostomy and avoid the duodenum and the annular pancreas [10].
4. CONCLUSION
Annular pancreas is a rare malformation that manifests itself primarily by signs related to duodenal stenosis. The diagnosis is currently based on abdominal CT scan and MRI of the pancreas. Treatment is exclusively surgical, and a by-passing procedure is the method of choice in the treatment of annular pancreas producing duodenal obstruction. Both the rarity of this congenital abnormality and its successful correction by surgical means have prompted us to make this presentation.
5. AUTHOR’S CONTRIBUTION
A Bouassria drafted the manuscript and revised it critically for content. H. Elbouhaddouti, O. Mouaqit, E. Benjelloun, A. Ousadden, K. Mazaz and K. Ait Taleb were the surgeons treating the patient and were involved in critically revising the draft for content.
NOTES
Competing interests: The authors declare that they have no competing interests.