
A heart transplant is a surgery in which a diseased heart is replaced with a healthy heart from a donor. Believe it or not, heart transplantation is a relatively simple operation for a cardiac surgeon.
There are three different types of heart transplants:
- The first operation is harvesting the heart from the donor.
- The donor is usually an unfortunate person who has suffered irreversible brain injury, called "brain death".
- Very often these are patients who have had major trauma to the head, for example, in an automobile accident. The victim's organs, other than the brain, are working well with the help of medications and other "life support" that may include a respirator or other devices.
- A team of physicians, nurses, and technicians goes to the hospital of the donor to remove donated organs once brain death of the donor has been determined. The removed organs are transported on ice to keep them alive until they can be implanted.
- For the heart, this is optimally less than six hours. So, the organs are often flown by airplane or helicopter to the recipient's hospital.
- The second operation is removing the recipient's damaged heart.
- Removing the damaged heart may be very easy or very difficult, depending on whether the recipient has had previous heart surgery (as is often the case).
- If there has been previous surgery, cutting through the scar tissue may prolong and complicate removal of the heart.
- The third operation is probably the easiest; the implantation of the donor heart.
- Today, this operation basically involves the creation of only five lines of stitches, or "anastomoses". These suture lines connect the large blood vessels entering and leaving the heart.
- Remarkably, if there are no complications, most patients who have had a heart transplant are home about one week after the surgery.
- The generosity of donors and their families makes organ transplantation possible.
History of the heart transplant
- The idea of replacing a bad organ with a good one has been documented in ancient mythology. The first real organ transplants were probably skin grafts that may have been done in India as early as the second century B.C.
- The first heart transplant in any animal is credited to Vladimer Demikhov. Working in Moscow in 1946, Demikhov switched the hearts between two dogs. The dogs survived the surgery.
- The first heart transplant in human beings was done in South Africa in 1967 by Dr. Christiaan Barnard; the patient only lived 18 days.
- Most of the research that led to successful heart transplantation took place in the United States at Stanford University under the leadership of Dr. Norman Shumway.
- Once Stanford started reporting better results, other centers started doing heart transplants. However, successful transplantation of a human heart was not ready for widespread clinical application until medications were developed to prevent the recipient from "rejecting" the donor heart. This happened in 1983 when the Food and Drug Administration (FDA) approved a drug called cyclosporine (Gengraf, Neoral).
- Before the advent of cyclosporine, overall results of heart transplants were not very good.
Who needs a heart transplant?
- There are not enough donor hearts available for everyone who may need a heart transplant. Therefore, there is a careful selection process in place to assure that hearts are distributed fairly and to those who will benefit most from the donor heart.
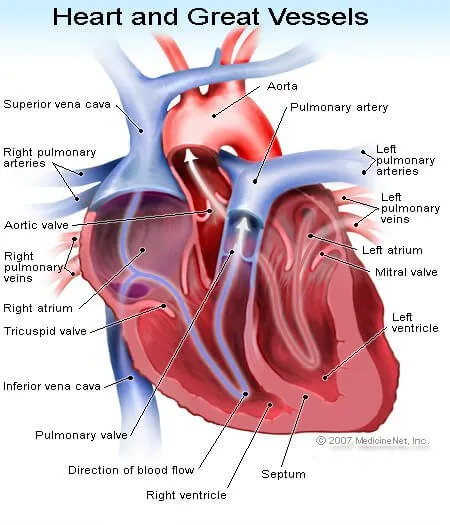
- The heart is just a pump, although a complicated pump. Most patients require a transplant because their hearts can no longer pump well enough to supply blood with oxygen and nutrients to the organs of the body.
- A smaller number of patients have a good pump, but a bad "electrical conduction system" of the heart. This electrical system determines the rate, rhythm and sequence of contraction of the heart muscle. There are all kinds of problems that can occur with the conduction system, including complete interruption of cardiac function causing sudden cardiac death.
- While there are many people with "end-stage" heart disease with inadequate function of the heart, not all qualify for a heart transplant. All the other important organs in the body must be in pretty good shape. Transplants cannot be performed in patients with active infection, cancer, or bad diabetes mellitus; patients who smoke or abuse alcohol are also not good candidates.
- It's not easy to be a transplant recipient. These patients need to change their lifestyle and take numerous medications (commonly more than 30 different medications). Hence, all potential transplants patients must undergo psychological testing to identify social and behavioral factors that could interfere with recovery, compliance with medications, and lifestyle changes required after transplantation.
- Moreover, needing a heart and being a suitable candidate are not enough. The potential donor heart must be compatible with the recipient's immune system to decrease the chance of problems with rejection.
- Finally, this precious resource, the donor organ, must be distributed fairly. The United Network for Organ Sharing (UNOS) is in charge of a system that is in place to assure equitable allocation of organs to individuals who will benefit the most from transplantation. These are usually the sickest patients.

QUESTION
What is heart failure? See AnswerWhat is the survival rate of a heart transplant?
- When all potential problems are considered, the results of transplantation are remarkably good. Keep in mind that heart failure is a very serious and life-threatening disease.
- In patients with severe forms of heart failure that require transplantation, the one year mortality rate (that is the percent of patients who die in within one year) is 80%.
- Overall, five-year survival in patients with any form of heart failure is less than 50%. Compare these outcomes with the cardiac transplant.
- After a heart transplant, five-year survival averages about 50%-60%. One year survival averages about 85%-90%.
What are the complications of a heart transplant?
- One might ask, "Why is survival no better than it is after a heart transplant?" As part of our defense mechanism to fight off infection and even cancer, our bodies have an "immune system" to recognize and eliminate foreign tissues such as viruses and bacteria.
- Unfortunately, our immune system also attacks transplanted organs. This is what happens when organs are rejected; they are recognized as foreign by the body.
- Rejection can be controlled with powerful "immunosuppressive" medications. If there is not enough immunosuppression the organ can reject acutely. Even when it seems that there is no active rejection, there may be more subtle chronic rejection that consists of growth of tissue, something like scar tissue, which causes blockage of the blood vessels of the heart.
- The blockage of the vessels is the process that ultimately causes the transplanted heart to fail. It is this chronic rejection that is the major limiting factor for the long-term success of heart transplantation.
- Unfortunately, immunosuppression is a double-edged sword. While immunosuppression blocks rejection, because it suppresses the immune system, transplant patients are more susceptible to infection and cancers of various types.
- Among older transplantation patients, as survival has improved, more patients are eventually dying from cancers.
Health News
- More of America's Pets Are Overdosing on Stray Coke, Meth
- GLP-1 Zepbound Is Approved As First Drug For Sleep Apnea
- Feeling Appreciated by Partner is Critical for Caregiver's Mental Health
- Tips for Spending Holiday Time With Family Members Who Live with Dementia
- The Most Therapeutic Kind of Me-Time
 More Health News »
More Health News »
What are the symptoms of a heart transplant rejection?
This is not an easy question to answer because many of the symptoms and signs of rejection and infection are the same. These include:
- weakness,
- fatigue,
- malaise (feeling lousy),
- fever, and
- "flu-like symptoms", such as chills, headaches, dizziness, diarrhea, nausea and/or vomiting.
The more specific symptoms and signs of infection will vary greatly depending upon the site of infection within the body. Transplant patients who experience any of these findings need to seek medical attention immediately.
The transplant physician will then do tests to determine whether the transplanted heart is functioning normally or not. If there is no evidence of rejection, a thorough search for infection will be performed so that the patient can be treated appropriately.
How is rejection of the heart transplant diagnosed and monitored?
- Currently, the gold standard for monitoring rejection is the endomyocardial biopsy. This is a simple operation for the experienced cardiologist and can be done as an outpatient procedure.
- First, a catheter is put into the jugular vein in the neck. From there, the catheter is advanced into the right side of the heart (right ventricle) using an x-ray method called fluoroscopy for guidance.
- The catheter has a bioptome at its end, a set of two small cups that can be closed to pinch off and remove small samples of the heart muscle. The tissue is processed and placed on glass slides to be reviewed under the microscope by a pathologist. Based on the findings, the pathologist can determine whether or not there is rejection.
- Immunosuppressive therapy is then adjusted, for example, increased if rejection is present. Investigators have tried to develop less invasive methods to monitor for rejection.
- There is a new high-tech analysis that can be done in a sample of blood that is very promising and much easier for the patient than the endomyocardial biopsy. This test looks at the expression of specific genes in cells in the blood. The amount of expression of key genes indicates whether or not rejection is occurring. While this method has not replaced the endomyocardial biopsy as the gold standard, it has decreased the frequency of biopsies for many patients.
Why are heart transplants not used more?
- It's not easy to qualify for a heart transplant. One has to have a very bad heart but an otherwise healthy body. However, the major limiting factor is the availability of donor hearts.
- For many reasons, individuals and families refuse to donate organs that could be life-saving to others. Sometimes, even when an organ is available, there is no good match. Other times, there is no way to get the heart to a suitable recipient in time for the organ to still be viable. Cost is another reason, although less frequent, why more heart transplants aren't done.
- The cost is always at least a few hundred thousand dollars. Not all insurers will pay for a heart transplant. The longer the recipient lives, the more expensive the transplant. Of course, if the heart lasts longer, the benefit is also greater to the patient and to society.
Subscribe to MedicineNet's Heart Health Newsletter
By clicking "Submit," I agree to the MedicineNet Terms and Conditions and Privacy Policy. I also agree to receive emails from MedicineNet and I understand that I may opt out of MedicineNet subscriptions at any time.
Top Heart Transplant Related Articles

Congestive Heart Failure (CHF)
Congestive heart failure (CHF) refers to a condition in which the heart loses the ability to function properly. Heart disease, high blood pressure, diabetes, myocarditis, and cardiomyopathies are just a few potential causes of congestive heart failure. Symptoms of congestive heart failure may include fatigue, breathlessness, palpitations, angina, and edema.
Coronary Angiogram
Coronary angiogram is an angiogram (an X-ray image of blood vessels filled with contrast material) used to diagnose coronary artery disease responsible for heart attacks, strokes, angina, and other coronary artery diseases. Coronary angiogram assists the physician in diagnosing and recommending treatment for coronary artery disease.
Plastic Surgery Pics
Thinking about getting plastic surgery? Check out before and after pictures of popular plastic surgery procedures, including: liposuction, tummy tuck, breast implants, rhinoplasty (nose job), neck lift, and more.
What Is the Difference Between Electrocardiogram and Electrocardiograph?
An electrocardiogram or electrocardiograph (ECG or EKG) are the same thing. An EKG is a test that examines the heart function by measuring the electrical activity of the heart. Based on the electrocardiogram, the doctor determines whether the electrical activity of the heart is normal or irregular, aiding in diagnosis of various heart problems.
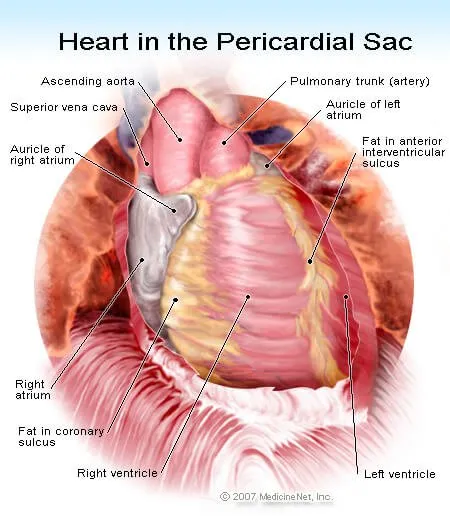
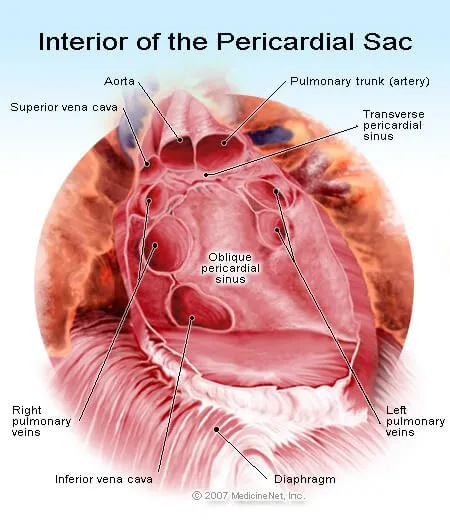
Heart Detail Picture
The heart is composed of specialized cardiac muscle, and it is four-chambered, with a right atrium and ventricle, and an anatomically separate left atrium and ventricle. See a picture of Heart Detail and learn more about the health topic.
How the Heart Works
The heart is a very important organ in the body. It is responsible for continuously pumping oxygen and nutrient-rich blood throughout your body to sustain life. It is a fist-sized muscle that beats (expands and contracts) 100,000 times per day, pumping a total of five or six quarts of blood each minute, or about 2,000 gallons per day.
Apheresis (Hemapheresis, Pheresis)
Apheresis (hemapheresis, pheresis) is a process of removing a specific component from the blood of a donor or patient that contains disease-provoking elements. Forms of apheresis include:- plasmapheresis,
- plasmapheresis,
- leukapheresis or leukopheresis,
- lymphopheresis or lymphapheresis, and
- erythropheresis.
- myasthenia gravis,
- lupus,
- severe rheumatoid arthritis,
- polymysositis,
- vacuities, and more.

How Is A Sternotomy Done?
A sternotomy is a surgical incision made through the breastbone (sternum) to access the thoracic cavity. A median sternotomy is the primary approach used for major surgeries in the thoracic region, as it offers a wide view.
Shock (Medical)
What is shock? A life-threatening condition with symptoms like low blood pressure, weakness, shallow breathing, clammy skin, fainting, anxiety, confusion, and chest pain. Learn about causes, types, and treatment.
Sudden Cardiac Arrest
Sudden cardiac arrest is an unexpected, sudden death caused by sudden cardiac arrest (loss of heart function). Treatment of sudden cardiac arrest is an emergency, and action must be taken immediately.
Vancomycin-Resistant Enterococci (VRE)
Vancomycin-resistant enterococci (VRE) infection is the most common type of infection acquired by patients while hospitalized. VRE are enterococci that have become resistant to the antibiotic vancomycin. There are only a few antibiotics that are able to treat VRE infections. However, newer antibiotics are being developed.
What Are The Four Heart Sounds?
Heart sounds are generated by blood flowing in and out of the heart’s chambers through the valves as they open and close. Listening to the heart sounds through a stethoscope (auscultation) is one of the first steps a physician takes in evaluating a patient’s medical condition. Heart sounds provide the doctor valuable information about heart function. Auscultation is used to detect abnormal heart sounds and decide on further course of action.