What is a hiatal hernia?

The esophagus connects the throat to the stomach. It passes through the chest and enters the abdomen through a hole in the diaphragm called the esophageal hiatus. The term hiatal hernia describes a condition where the upper part of the stomach normally located just below the diaphragm in the abdomen pushes or protrudes through the esophageal hiatus to rest within the chest cavity.
What are the types of hiatal hernias?
There are three types of hiatal hernias.
- Sling hiatal hernia: A sliding hiatal hernia is the most common type of hiatal hernia is a sliding hiatal hernia.
- A sliding hiatal hernia accounts for 95% of all hiatal hernias.
- In a sliding hernia, a portion of the stomach slides upward through the diaphragm and into the chest such that the junction of the esophagus and stomach (gastroesophageal junction) lies in the chest.
- A sliding hernia is present during inspiration when the diaphragm contracts and descends toward the abdominal cavity and when the esophagus shortens during swallowing, but at rest, it is not present.
- Paraesophageal hernia: A paraesophageal hernia accounts for only 5% of hiatal hernias, the gap in the diaphragm through which the hernia occurs, phrenoesophageal membrane is larger, and a portion of the stomach herniates into the chest alongside the esophagus and stays there, but the junction between the stomach and the esophagus remains below the diaphragm.
- Paraesophageal and sliding: In a combination of events, should the defect in the diaphragm become larger, the junction between the stomach and the esophagus can herniate through the diaphragm into the chest causing a hernia that is both paraesophageal and sliding.
What causes a hiatal hernia?
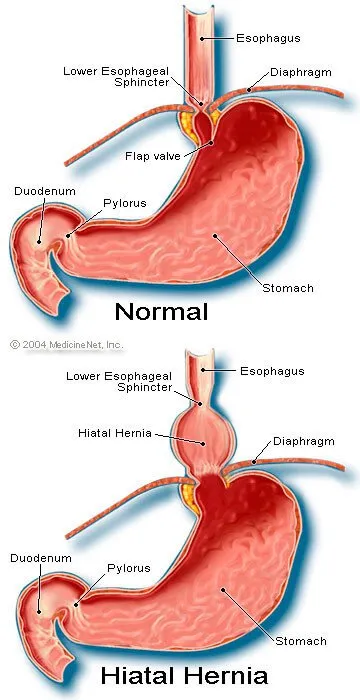
Normally, the space where the esophagus passes through the diaphragm is sealed by the phrenoesophageal membrane, (a thin membrane of tissue connecting the esophagus with the diaphragm) where the esophagus passes through the diaphragm. Thus, the chest cavity and abdominal cavity are separated from each other. Because the muscles of the esophagus tighten and the esophagus shortens with each swallow, essentially squeezing food into the stomach, this membrane needs to be elastic to allow the esophagus to move up and down.
Normal physiology allows the gastroeophageal junction, where the esophagus and stomach meet, to move back and forth within the hiatus. However; at rest, the gastroeophageal junction should be located below the diaphragm and in the abdominal cavity. It is important to remember that these distances are very short.
Over time, the phrenoesophageal membrane may weaken, and a part of the stomach may herniate through the membrane. It may remain above the diaphragm permanently or move back and forth across the diaphragm.
Hiatal hernias are common, and in the majority of cases, the cause is unknown. They may be present at birth or develop later in life.
- Pregnancy: Theoretically, decreased abdominal muscle tone and increased pressure within the abdominal cavity could lead to the development of a hiatal hernia. Thus, people who are obese and women who are pregnant may be at an increased risk for developing a hiatal hernia although this has not been demonstrated.
- Constipation and vomiting: People who have repetitive vomiting or those who have constipation and strain to have a bowel movement, increase the intra-abdominal pressure when they strain, and this may weaken the phrenoesophageal membrane.
- The membrane also may weaken and lose its elasticity as a part of aging.
- Ascites: Ascites is an abnormal collection of fluid in the abdominal cavity, which is often seen in people with liver failure, and also may be associated with the development of a hiatal hernia.

QUESTION
Bowel regularity means a bowel movement every day. See AnswerWhat does a hiatal hernia feel like?
Hiatal hernias do not cause symptoms, and most are found incidentally when a person has a chest X-ray or abdominal X-rays, including:
- An upper GI series and CT scans in which the patient swallows barium or another contrast material.
- It also is found incidentally during gastrointestinal endoscopy of the esophagus, stomach, and duodenum (EGD).
- If symptoms do occur, they are due to gastroesophageal reflux disease (GERD) where the digestive juice containing acid from the stomach moves up into the esophagus.
Unfortunately, the esophagus does not have a similar protective lining. Instead, it relies on the lower esophageal sphincter (LES), a band of muscle located at the junction of the stomach and esophagus, and the muscle of the diaphragm surrounding the esophagus to act as a valve to prevent acid from refluxing from the stomach into the esophagus.
Moreover, to the esophageal sphincter (LES), the normal location of the stomach and esophageal junction within the abdominal cavity is important in keeping acid where it belongs. There is increased pressure within the abdominal cavity compared to the chest cavity, particularly during inspiration which would normally cause the acid and contents from the stomach to reflux back into the esophagus, but the combination of the pressure exerted within the lower mostly is from the esophageal sphincter (LES), and the muscle of the diaphragm create a zone of higher pressure that keeps stomach acid in the stomach.
In the situation of a sliding hiatal hernia, the gasatroesophageal and esophagus junction move above the diaphragm and into the chest, and the portion of the higher-pressure zone due to the diaphragm is lost. Acid is allowed to reflux back into the esophagus causing inflammation of the lining of the esophagus.
The symptoms of gastroesophageal reflux disease (GERD) include:
- Heartburn
- Chest pain or burning
- Nausea
- Vomiting or retching (dry heaves)
- Burping
- Waterbrash (rapid appearance of a large amount of saliva in the mouth that is stimulated by the refluxing acid)
What makes symptoms of a hiatal hernia more painful and worse?
- Symptoms of a hiatal hernia usually are worse after meals and may be made worse when lying flat, which may resolve with sitting up or walking.
- In some people with a hiatal hernia, it refluxes into the lower esophagus which sets off nervous reflexes that can cause a cough or even spasm of the small airways within the lungs people.
- Rarely, some people with a hiatal hernia may feel a reflux of acid droplets into the back of their throat. This acid can be inhaled or aspirated into the lung causing:
- Coughing spasms
- Asthma
- Repeated lung infections including pneumonia and bronchitis
People of any age can get a hiatal hernia from infants to the elderly. Fortunately, it is very rare.
What is a paraesophageal hiatal hernia? What are its symptoms and signs?
Usually, people with a paraesophageal sphincter have no symptoms of reflux because the gastroeophageal esophagus junction remains below the diaphragm, but if the hernia is large, the way the stomach rotates into the chest, there is the possibility of volvulus of the stomach in which the stomach twists upon itself. Fortunately, paraesophageal hernias are relatively uncommon.
Rarely, gastric volvulus of the stomach in which an abnormal rotation of the stomach more than 180 degrees is a surgical emergency and causes difficulty with the following:
- Painful swallowing
- Chest pain
- Vomiting
Health News
- More of America's Pets Are Overdosing on Stray Coke, Meth
- GLP-1 Zepbound Is Approved As First Drug For Sleep Apnea
- Feeling Appreciated by Partner is Critical for Caregiver's Mental Health
- Tips for Spending Holiday Time With Family Members Who Live with Dementia
- The Most Therapeutic Kind of Me-Time
 More Health News »
More Health News »
What procedures and tests diagnose hiatal hernias?
- X-rays, EDG, and CT scan: Most often, a hiatal hernia is found incidentally with gastrointestinal X-rays, EGD, and sometimes CT scans, since by itself, it causes no symptoms. When there are associated symptoms of GERD, they usually need treatment. With symptoms of GERD, a hiatal hernia is likely to present since most people with GERD have hiatal hernias.
- Barium swallow or upper GI series: Often, the diagnosis of a hiatal hernia is confirmed by a barium swallow or upper GI series, where a radiologist uses fluoroscopy to observe in real-time as the swallowed barium outlines the esophagus, stomach, and upper part of the small intestine. In addition to seeing the anatomy, the radiologist also can comment upon the movement of the muscles that work to propel the barium (and presumably) food through the esophagus into the stomach and beyond.
- Endoscopy: Endoscopy is a procedure performed under sedation by a gastroenterologist to look at the lining of the esophagus, stomach, and duodenum. A hiatal hernia may be diagnosed easily in this manner and more importantly, the physician may be able to see complications of GERD from the reflux of acid. Endoscopy is used to diagnose scarring with strictures (narrowing of the esophagus) and precancerous conditions like Barrett's esophagus. Biopsies or small tissue samples may be taken and examined under a microscope.
What is the treatment for hiatal hernias?
The treatment for hiatal hernia is actually the treatment for GERD and minimizing acid reflux, such as:
- Decreasing acid secretion in the stomach
- Avoiding substances that are irritating to the stomach lining
- Mechanical means to keep the remaining acid in the stomach where it belongs
What medications treat hiatal hernias?
Proton pump inhibitor (PPI) medications are commonly used to decrease acid production, which include:
When is surgery for a hiatal hernia necessary?
Most often, the surgery is done as a minimally invasive procedure using a laparoscope. While there are different techniques, the results are similar and the best option is usually the one the surgeon feels most comfortable performing in a specific situation.
- Proton pump inhibitor medications: With the development of proton pump inhibitor medications, medical therapy has decreased the necessity of surgery for sliding hiatal hernias, and it is often only recommended for people who have failed aggressive drug treatment or who have developed complications of GERD including:
- Paraesophageal hernias: People with paraesophageal hernias often have no symptoms, and surgery is required only if the hernias become trapped in the chest and become stuck in the diaphragmatic hiatus or rotate to cause a volvulus. While this is more commonly seen in older people, paraesophageal hernias also may occur from birth as a congenital condition in neonates and infants.
Subscribe to MedicineNet's Daily Health News Newsletter
By clicking Submit, I agree to the MedicineNet's Terms & Conditions & Privacy Policy and understand that I may opt out of MedicineNet's subscriptions at any time.
What are the complications of a hiatal hernia? Is it serious?
If treated, a hiatal hernia is appropriate and lifestyle changes are made, you can minimize the effects of a hiatal hernia. If left untreated, complications can cause a strangulated hiatal hernia, which symptoms include:
- They won't go away
- Are severe
- You are not clear on what is causing your symptoms
Signs and symptoms of a hiatal hernia that needs to be treated right away, include:
- Vomiting blood
- Dark, tarry stools
- Palpitations (feel the heart beating in your chest) or feeling faint
- Cough and fever
- Shortness of breath
- Inability to swallow solid food or liquids easily
- Chest pressure or pain, especially if you know that you have heart disease or these risk factors:
- diabetes,
- smoking,
- high cholesterol,
- high blood pressure,
- older than 55 years,
- male gender, or
- family history of early heart attacks or angina (before age 55 years).
A strangulated hernia is a medical emergency. If you have any of these symptoms call 911 or go to your nearest Emergency Department.
What diet changes help avoid hiatal hernia pain, symptoms, and triggers?
Foods, drinks, and home changes that treat hiatal hernia symptoms include:
- Elevating the head of the bed when sleeping allows gravity to prevent acid from refluxing into the esophagus.
- Eating small frequent meals may help instead of eating two or three larger meals a day.
- Some foods that trigger hiatal symptoms should be avoided, which include:
- Spicy
- Greasy foods
- Onions
- Tomatoes
- Citrus fruits
However, most people are generally aware of the foods that trigger heartburn symptoms and avoid them.
Society of American Gastrointestinal and Endoscopic Surgeons. Guidelines for the Management of Hiatal Hernia.
Top Hiatal Hernia Overview Related Articles

Can You Heal a Hernia Without Surgery?
While non-surgical approaches such as wearing a corset, binder, or truss may exert gentle pressure on the hernia and keep it in place, a hernia usually does not go away without surgery. Conservative or non-surgical management should strictly be done under a doctor’s supervision because they may lead to complications such as bowel obstruction and strangulation.
Endoscopy
Endoscopy is a broad term used to describe examining the inside of the body using a lighted, flexible instrument called an endoscope. Endoscopy procedure is performed on a patient to examine the esophagus, stomach, and duodenum; and look for causes of symptoms such as abdominal pain, nausea, vomiting, difficulty swallowing, or intestinal bleeding.
Esophagitis
Esophagitis is caused by an infection or irritation of the esophagus. Infections that cause esophagitis include a candida yeast infection of the esophagus as well as herpes. Signs and symptoms of esophagitis include cough, mouth sores, chest pain, bad breath, sore throat, heartburn, and difficulty swallowing. Treatment of esophagitis includes diet, lifestyle changes, and medication depending upon the cause.
Gastroesophageal Reflux Disease (GERD)
Gastroesophageal reflux disease (GERD), also called acid reflux, can cause symptoms like heartburn, chest pain, regurgitation, and nausea. Learn about causes, diagnosis, treatment and prevention.
GERD Quiz
Who is at risk for developing GERD? Are you? Take this quiz to learn what GERD is, if you're at risk, and what you can do about it.
Heartburn
Heartburn is a burning sensation experienced from acid reflux (GERD). Symptoms of heartburn include chest pain, burning in the throat, difficulty swallowing, the feeling of food sticking in the throat, and a burning feeling in the chest. Causes of heartburn include dietary habits, lifestyle habits, and medical causes. Treatments for heartburn include lifestyle changes, OTC medication, prescription medication, and surgery.
Heartburn Foods Slides
Learn the symptoms of heartburn and which foods cause heartburn or GERD. Discover home remedies and which foods may provide treatment for heartburn relief.
Hernia
A hernia occurs when an organ or piece of tissue protrudes from the space in which it is normally contained. Symptoms of a hernia include pain, nausea, vomiting, bowel obstruction, and fever. Hernias are diagnosed by a physical exam and imaging tests. Some hernias may be held in place with a supportive belt. Other hernias require surgical repair. The prognosis of people who undergo elective hernia repair tends to be good.
Hernia Quiz: Test Your Medical IQ
Exactly what is a hernia and why do we get them? Take this quiz to learn causes, symptoms, treatments and home remedies for this common condition.
Hernias: Causes, Types, and Treatments
Hernias often don't cause many symptoms, but they can lead to some serious problems. Use this WebMD slideshow to help yourself learn about what to look for and how they’re treated.
How Long Does It Take to Recover from Laparoscopic Inguinal Hernia Surgery?
A laparoscopic inguinal hernia repair is a routine surgery to repair a weakness or perforation in the muscle or tissue in the abdominal cavity. Most people can return to normal activities in two weeks, but may need to avoid heavy lifting.
How Long Does It Take to Recover From Incisional Hernia Surgery?
An incisional hernia is a type of hernia caused by an incompletely healed surgical wound. In an incisional hernia, the intestine pushes through the abdominal wall from the site of previous abdominal surgery. Incision hernia is mostly seen in elderly or overweight people who are inactive after abdominal surgery.
What Is the Recovery Time for An Umbilical Hernia Surgery?
An umbilical hernia repair is a relatively routine surgery and takes about 20 to 30 minutes. It can be performed as an open surgery or a minimally invasive laparoscopic surgery. An open surgery might require two to three days of hospitalization, but with a laparoscopic surgery a patient may be able to go home the same day or after 24 hours.
Stomach Picture
The stomach is a muscular sac located on the left side of the upper abdomen. See a picture of the Stomach and learn more about the health topic.
The Digestion Process
Digestion is the complex process of turning the food you eat into the energy you need to survive. The digestive process also involves creating waste to be eliminated and is made of a series of muscles that coordinate the movement of food. Learn more about digestion and the body parts that make it possible, including the mouth, pharynx, esophagus, stomach, small intestine, colon, rectum, anus, pancreas, liver, and gallbladder.
