How Is a Migraine Headache Different?

While 30 million Americans suffer from it, migraine is still surprisingly misunderstood. People with migraine suffer in unapparent ways, making this an invisible disease.
Migraine headaches can be famously painful, but migraine is more than just a headache. An estimated 50% of those with migraine have never been diagnosed, or have been improperly diagnosed as having another type of headache. Knowing what kind of headache you have can help you find relief through proper treatment.
The type of headache associated with migraine is throbbing and at least moderately painful—at least a “5” on a scale from 1-10. This headache will last from 4 to 72 hours. It is usually felt only on one side of the head, often behind one eye. And it may be initiated or "triggered" by specific compounds or situations (stress, hormones, foods, and many others).
Women have it about three times more often than men. While these painful headaches get plenty of attention, what mostly distinguishes a migraine attack from any other headache type are the sensory symptoms discussed on the next slide.
Other Symptoms

Migraine headaches—throbbing pain, usually on only one side of the head—can be intense enough to prevent you from completing simple tasks or working. But the accompanying sensory symptoms can also derail your day. And they tend to be a little different for every person. While we commonly talk about the headaches involved, some people with migraine do not get headaches.
Migraine attacks can cause vision problems and nausea. Certain smells, sounds, or light levels may become painful. The pain can be so severe that basic tasks and movements become difficult. More than 50% of patients say that they are less productive at home or at their jobs during an attack.
The headache pain may radiate toward your eyes, forehead, or temple and cause nausea, vomiting, vision problems, or oversensitivity to normal light or mild exertion. You may also experience muscle tenderness and pain from light touch.
With or Without Aura?

Not all migraine cases are the same. One way to distinguish them is to determine whether or not you experience an aura. So-called "complicated" migraine attacks begin with an aura. These can be visual distortions such as dots, wavy lines, or zig zags. Some people experience numbness or tingling across one side of the body. If they accompany headaches, auras usually appear about an hour earlier. If they do not, these auras are called "ocular migraines." Some people experience migraine headache aura without pain.
About a quarter of people diagnosed with migraine ("migraineurs") have this type. For those who do not, their condition is known by professionals as "common migraine." Even without aura, you may experience light sensitivity, nausea, and other symptoms.
Warning Signs

"Classic" auras do not occur in all patients, but about 25% of patients can have a prodromal phase—an early stage that begins with mild symptoms. The prodromal phase occurs as long as 24 hours before pain develops. Some experience mood changes (depression, excitability, irritability) and sensations of odd smells or tastes, while others may feel tired or tense.
What Causes Migraine Attacks?
Migraine headache causes are complex. Though it is the world's most common cause of neurological disability, researchers are only beginning to understand what causes migraine. One common explanation was recently thrown out. This is the so-called vascular theory, which was proposed in 1938. It claims that pressure changes in the vascular system near the brain cause migraine. But after testing, this theory is no longer considered valid. Migraine is now considered a gene-related neurological disease, and not a vascular one.
Current research shows a variety of genetic mutations are at least partly responsible. The gene TRESK has been identified as the site of one such genetic mutation. The TRESK gene provides the blueprints for a potassium ion channel that is believed to help your nerve cells rest. When mutations occur in this gene, they may cause nerve cells to become overexcited, making them more responsive to less pain.
Although gene mutations tell part of the story, migraine initiation is enormously complicated. It relies on several processes which either result in a visibly changed brain structure or are caused by these structural changes. In fact, some scientists believe there is not a single cause, but rather multiple causes at play. Research continues in this growing field.
Trigger: Flashing Lights

Migraine headaches are often triggered to occur when the person is exposed to a specific set of circumstances. One of the most common triggers is strong flickering light. For example, faulty fluorescent lights, a television picture rapidly going on and off, or sunlight reflected off of waves in a lake or the ocean are all potential triggers; there are many others.
Trigger: Anxiety and Stress
As mentioned, stress is sometimes a trigger. While it is unlikely that people can live stress-free lives, many people can reduce their stress and avoid triggering attacks by using relaxation techniques, deep breathing, and other biofeedback techniques.
Trigger: Lack of Food or Sleep

Regular daily patterns of meals and sleep work well for some individuals to avoid attacks. Sleep interruptions and lack of adequate fluid and/or food intake and even some food binges may trigger them.
Trigger: Hormonal Changes

Many women's attacks are linked to their menstrual cycle. The hormonal increases and decreases are thought to be responsible in some women. However, patterns differ from person to person so one type of hormonal therapy may benefit one woman, but it may be unhelpful or even increase migraine symptoms in other women.
Trigger: Headache Foods

Although studies have not proven that any food is a migraine trigger, patients often suggest certain foods trigger them. Common migraine headache trigger foods or food ingredients cited by patients are red wine, cheese, chocolate, soy sauce, processed meat, and MSG.
Trigger: Tyramine

When it comes to migraine headache triggers, tyramine is near the top of the list. Tyramine, produced from the amino acid tyrosine, may be a trigger because it can cause blood vessel constriction and expansion. Many aged and fermented foods that are associated with attacks contain tyramine, like cheeses, soy sauce, pickles, and aged meats like pepperoni.
Caffeine: Help or Hindrance?

The caffeine in coffee may help relieve attacks when used with some medications. However, when the caffeine levels drop, the patient may then be prone to develop headaches. Consequently, it may be both a help and a hindrance.
Tracking Personal Triggers
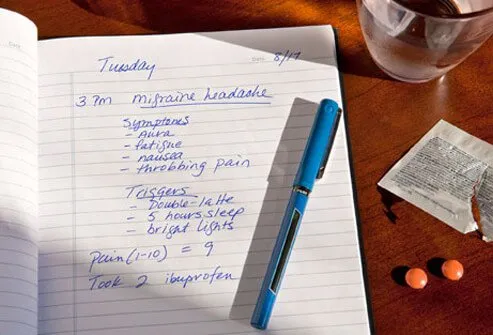
Individuals should keep a diary or list of things that act as warning signs or triggers of an oncoming migraine. This information may help migraine sufferers to avoid future attacks.
Who Has Migraine?

Who gets migraine headache? Attacks occur in women about three times more often than in men. People with relatives who get them are more likely to as well. In addition, attacks occur more often in people with epilepsy, depression, stroke, asthma, anxiety, and in individuals with neurologic and hereditary (genetic) disorders.
Migraine in Children

Migraine episodes occur in children about equally until puberty when attacks become more common in girls. However, in children, migraine symptoms are somewhat different than those in adults; children may experience stomach pains (abdominal migraine), frequent and forceful vomiting, or benign paroxysmal vertigo where the symptoms are unsteady balance, involuntary eye movements, vomiting, and behavioral changes.
Diagnosing Migraine

Migraine is usually diagnosed based on a clinical history of your symptoms. However, most doctors will do a CT or MRI brain scan to determine if other causes of headaches (brain tumor or bleeding into the brain, for example) are present. Migraine headache diagnostic criteria are used to establish the diagnosis of migraine.
Non-Migraine Headaches

Do you have a migraine headache or a sinus or tension headache? Or is it something else? “Something else” usually means one of the two commonly diagnosed headache types discussed below. However, migraine experts warn that many people diagnosed with these headaches are actually migraineurs. Roughly half of all people with migraine in the US are thought to be undiagnosed, and mistaken diagnosis of these headaches may prevent you from receiving the care you need.
Although becoming familiar with other types of headaches may help you find relief, it can be tricky to get the right diagnosis. That’s because these various headache types share many of the same symptoms, and because no definitive test has been developed to test for them. Some experts have begun to describe all of these headaches as part of a continuum, with occasional, mild tension headache on one side, and chronic migraine headaches on the other.
Tension Headaches
Are your shoulders and neck tense? It’s a common problem that sometimes leads to chronic headaches. Tension headaches are defined as mild to moderate in terms of pain. You can feel these headaches around your head, but especially the back of your head and forehead. They usually cause no other symptoms.
Sinus Headaches
Sinus headaches are described as mild to moderate pain in the places near your sinuses—your cheeks, eyes, and across your nose. These headaches require the patient to first have a sinus infection. Often a seasonal condition, these headaches are rarely chronic. Doctors are encouraged to test the immune system if more than one bacterial sinus headache is confirmed in a single year.
Calculating Your Headache Burden
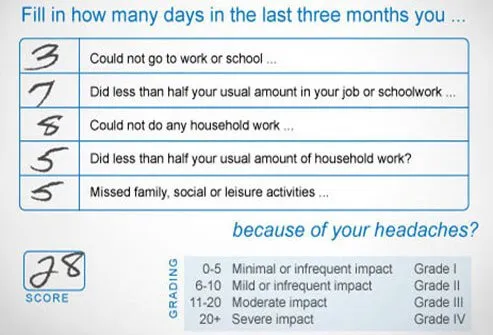
Some doctors like to estimate how much migraine disrupts normal activities before treatment begins. A questionnaire is given to the patient to estimate how often they miss various functions (school, work, family activities) because of their attacks.
Migraine Treatment: Over-the-Counter Drugs

There are many types of over-the-counter (OTC) medicines for headache pain. Some of the most common medications for headaches include nonsteroidal anti-inflammatory drugs. Aspirin, naproxen sodium, ibuprofen, and acetaminophen may provide relief. Anti-nausea medications like Dramamine may also be useful. Some OTCs are marketed as treatments for migraine. Although all of these OTCs may be helpful for some headache types, people should not overuse them to avoid toxicity, ulcers, and other gastrointestinal problems. In addition, overdoing it can lead to medication-overuse headaches that may make your attacks worse.
Treatment: Triptans

Triptans (Amerge, Axert, Frova, Imitrex, Maxalt, Relpax, Treximet, and Zomig) are the most commonly prescribed medication for the treatment of migraine. However, people with hypertension, heart disease, stroke, and those who take certain medications may not be able to take triptans; your doctor can help with medication choices. Unfortunately, side effects of nausea, dizziness, chest pain, and paresthesia may occur with triptans.
Treatment: Ergotamines

Ergotamines (Cafergot, Migergot, or Migranal) are some of the first medications created to treat migraine, and they are usually not as effective as triptans. They have side effects such as nausea, dizziness, muscle pain, or an unusual or bad taste in the mouth and may interact with other drugs. These side effects and drug interactions may limit the patient's use of the drug.
Novel Migraine Therapies: Gepants, Ditans, and More
Not long ago, the medications used to treat migraine were designed for other diseases such as hypertension and epilepsy. While these may still be useful for some individuals, a better understanding of how migraine works has led to more targeted drug therapies. Together, three new classes of pharmaceuticals are transforming migraine treatment.
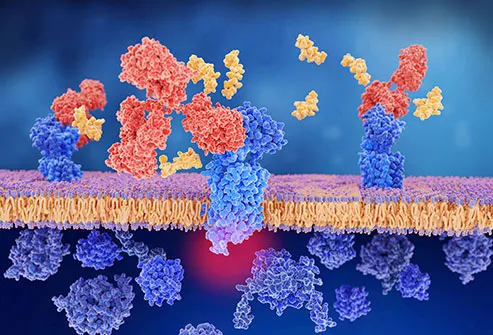
Gepants (small molecules that block CGRP) & Monoclonal Antibodies
Two of these new drug classes work by blocking a molecular structure known as CGRP (calcitonin gene-related peptide). CGRP is released during migraine attacks, and blocking it may stop the attack before it gets going. This may help your nerves relax.
To do this, gepants and monoclonal antibodies have been used. The first of these to receive FDA approval was Erenumab (Aimovig), followed soon by two more in the same year. These drugs may cause side effects, and the consequences of long-term use are unknown. So, discuss them thoroughly with your doctor. It may help if you bring a list of relevant questions on your visit.
Ditans
The ditan class of drugs work differently. They target a receptor (5-HT1F) found in different brain regions. By doing so, these drugs seem to reduce inflammation that arises in your nervous system. These drugs are still being tested, and seem to include side effects like drowsiness and vertigo. The first ditan, lasmiditan, was FDA approved in 2019.
Novel Migraine Therapies: Nerve Stimulation (Neuromodulation)

Can electrical devices stop headache pain cold? For some people they work well. Sometimes called electrical stimulation devices, these tools can alter brain activity—sometimes by stimulating activity, but more often by calming it in the case of migraineurs. The treatment is known more broadly as neuromodulation.
Some neuromodulation devices have been approved by the FDA for home use. Two devices attach to your head, while one is pressed against your throat to reach the vagus nerve. Other stimulators still in development can be implanted.
The advantage of these devices is that they can provide relief when medication use is hampered by side effects or contraindications. However, they have not taken off yet in the consumer market, perhaps due to their cost. They also seem to work better for some patients than for others.
Is Your Treatment Working?

Sometimes the initial treatments for migraine either do not reduce the symptoms or only marginally reduce them. If, after trying the prescribed treatment(s) about two or three times and getting little or no relief, you should ask your doctor to change the treatment. However, patients are urged to treat their attacks early (within about 2 hours) to get full benefit of treatments. It may take some trial and error to find the migraine headache treatment that works for you.
Limits of Medication Use

Some chronic headaches are due to overuse of medicine; avoid using migraine-prescribed medicines more than twice per week. Using and tapering medicine for migraine should proceed under your doctor's supervision. Narcotics are used as a last resort for migraine because they can be addictive.
Treatment: Vitamins and Supplements

Some vitamins and supplements may be useful therapies. Some of these are currently being tested. These are collectively known as nutraceuticals. The nutraceuticals that have shown some evidence of relief in preliminary testing include magnesium, riboflavin (vitamin B2), plus butterbur root extract and feverfew (herbals).
Treatment: Preventive Medicines

If your attacks are frequent and severe, your doctor may prescribe medication(s) to lessen the frequency or to prevent the headaches. Medicines that are used in this manner include Timolol (Blocadren), divalproex sodium (Depakote), propranolol (Inderal), and topiramate (Topamax), although the drugs were designed to reduce hypertension or prevent seizures.
Alternative Therapy: Biofeedback
Other methods that may reduce or prevent migraine include biofeedback techniques to reduce headache triggers like stress and early symptoms such as muscle tension.
Alternative Therapy: Acupuncture

Although studies on acupuncture are not definitive, some patients’ headaches may respond well to this Chinese method of inserting needles into specific body locations to reduce or stop pain. Because the results are so variable, some doctors do not recommend this treatment. But because some patients report headache relief, it is another treatment method to consider.
An Advantage of Aging

The peak intensity and frequency of attacks occur between ages 20 to 60. As you age past 60, migraine intensity and frequency of headache and related symptoms decreases, and in some patients, attacks cease.
When You Need Quick Care

Most people know the pattern of their attacks (triggers, auras, and headache pain intensity). However, new headaches, in people with or without a migraine history, that last about 2 or more days should be checked by a doctor. However, if a headache develops with symptoms such as fever, stiff neck, confusion, or paralysis, the person should be examined emergently. The person should be taken by their relative, friend, or caretaker to an Emergency Medicine Department.
Migraine or Tension Headache? Symptoms, Triggers, Treatments
This tool does not provide medical advice. See additional information: 
© 1996-2024 WebMD, LLC. All rights reserved.