What is primary biliary cirrhosis (PBC)?
Primary biliary cirrhosis (PBC) is a progressive disease of the liver caused by a buildup of bile within the liver (cholestasis) that results in damage to the small bile ducts that drain bile from the liver. Over time, this pressure build-up destroys the bile ducts leading to liver cell damage. As the disease progresses and enough liver cells die, cirrhosis and liver failure occur.
PBC can cause a range of symptoms, including fatigue, itching, dry eyes and mouth, abdominal pain, and jaundice (yellowing of the skin and eyes). Some people with PBC may have no symptoms at all, and the disease may be discovered incidentally during routine blood tests or imaging studies.
Bile is manufactured in the liver and then transported through the bile ducts to the gallbladder and intestine where it helps digest fats and fat-soluble vitamins (A, D, E, K). When bile cannot be drained from the liver, it causes inflammation that leads to cell death. Scar tissue gradually replaces the areas of the damaged liver and then the body cannot perform necessary functions.
What are the causes and risk factors of primary biliary cirrhosis?
The cause of PBC is unknown. It is most likely an autoimmune disease, where the body's immune system attacks its cells. In this disease, the bile ducts are under attack and are destroyed.
Risk factors for primary biliary cirrhosis
- There may be a genetic component to the development of PBC since a person with the disease is likely to have a family member also afflicted.
- Women are nine times more likely than men to develop PBC. It most often develops in middle age between the ages of 40 to 60.
- The disease is seen more often in white, northern Europeans, compared to African-Americans.
- Other autoimmune diseases: People with other autoimmune diseases, such as rheumatoid arthritis or Sjögren's syndrome, are at a higher risk of developing PBC.
- Environmental factors: Exposure to certain chemicals or infections may increase a person's risk of developing PBC.
What are the signs and symptoms for primary biliary cirrhosis?
Up to a quarter of patients with primary biliary cirrhosis are asymptomatic, meaning they do not have symptoms at the time of diagnosis and the disease is found incidentally because of abnormal liver blood tests.
The most common initial symptoms include:
- Fatigue or a sense of being abnormally tired
- Skin that itches
- Because of the intense itching and scratching, the skin may become darkened and discolored in some areas
- The person may also complain of dry mouth and eyes
- Bone and joint pain
- Easy bruising and bleeding
Because there may be liver inflammation, some people may experience right upper quadrant abdominal pain, where the liver is located.
Should the liver damage progress, the symptoms of cirrhosis may develop, such as:
- Muscle wasting
- Ascites (swelling of the abdomen due to fluid accumulation)
- Leg swelling
- Jaundice (yellow coloration of the skin)
- Confusion

SLIDESHOW
Hepatitis: Surprising Things That Can Damage Your Liver See SlideshowHow is the diagnosis of primary biliary cirrhosis made?
The diagnosis of primary biliary cirrhosis is considered when the doctor suspects that there might be liver inflammation based on the history and physical examination. Initially, there may be a few symptoms like itching or fatigue to help guide further testing
The diagnosis may be made incidentally when abnormal liver functions are found on routine blood tests drawn for another reason. Liver function tests include AST (aspartate aminotransferase), ALT (alanine aminotransferase), GGT (gamma-glutamyl transpeptidase), alkaline phosphatase, and bilirubin. Blood levels tend to become elevated in liver disease and they may rise in specific patterns depending upon the underlying cause of inflammation.
Once the diagnosis is suspected, a blood test to check for antimitochondrial antibodies (AMA) is usually done. This is positive in over 90% of patients with PBC.
Other blood tests may be considered including a complete blood count (CBC) and cholesterol levels.
Imaging of the abdomen by ultrasound, CT scan, or MRI is often considered to look for structural changes in the liver and to search for tumors.
A liver biopsy, where a thin needle is inserted through the skin to take a piece of liver tissue, may help confirm the diagnosis. This tissue is examined under a microscope by a pathologist to look for changes consistent with PBC. It is also useful to help stage the disease, deciding its severity at the time of diagnosis.
It's important to note that the diagnosis of PBC can be challenging, and it may take some time to reach a definitive diagnosis.
What is the treatment for primary biliary cirrhosis?
The treatment for primary biliary cirrhosis (PBC) aims to manage symptoms, slow the progression of the disease, and prevent complications.
Treatment options for PBC may include:
- The only "cure" for primary biliary cirrhosis is a liver transplant, but it is only considered as a treatment option if other less aggressive treatments have failed and the patient develops liver failure.
- Ursodiol (Actigal) or ursodeoxycholic acid (UDCA) is the first-line treatment for PBC. It helps the liver transport bile into the gallbladder and intestine, in an attempt to prevent cholestasis.
- Depending upon the severity of the disease, immune suppression medications may be prescribed, including methotrexate (Rheumatrex, Trexall), cyclosporine, and prednisone.
- Immunosuppressants: Immunosuppressant medications, such as azathioprine or mycophenolate, may be used to suppress the immune system and reduce inflammation in the liver.
- Itching may be intense and difficult to control. Antihistamines like diphenhydramine (Benadryl) may be helpful but other drugs may be considered including cholestyramine (Questran, Questran Light), which helps bind bile and decrease the itching associated with elevated bilirubin levels in the blood.
- Complications of PBC will need to be cared for. These include cirrhosis, portal hypertension, gastrointestinal bleeding, osteoporosis, and vitamin deficiencies.
What is the prognosis for someone with primary biliary cirrhosis?
PBC is a progressive disease that can be controlled but not cured. The prognosis depends upon a variety of factors including whether the patient has symptoms (especially fatigue), liver function test abnormalities, and whether the patient has undergone treatment with medication or has required liver transplantation.
Advances in treatment have extended life expectancy in the past many years.
The average survival from diagnosis for a patient with PBC who is asymptomatic is 16 years, while that of patients with symptoms is 7 1/2 years.
What are the complications of primary biliary cirrhosis?
The complications of primary biliary cirrhosis develop as the ability of the liver to function decreases. Cirrhosis describes liver scarring and failure. The liver is responsible for helping to digest food, producing proteins, blood clotting factors, and enzymes that help digest food.
Some complications include the following:
- Ascites: Fluid collection within the abdomen that occurs because the liver cannot produce enough albumin, a protein that helps keep fluid within the blood vessels. Ascites fluid is prone to infection and a condition called spontaneous bacterial peritonitis (peritoneum=sac that contains the abdominal organs + itis=inflammation)
- Edema: Swelling of the legs may occur, again because of decreased albumin levels in the body
- Easy bruising or bleeding: The liver is responsible for producing blood clotting factors. Without an adequate supply, there is an increased risk of bleeding. Patients may have a low platelet count because of an enlarged spleen causing easy bruising.
- Hepatic encephalopathy: The liver also helps remove waste products from the bloodstream. Ammonia is the chemical waste product of protein metabolism and the body requires a healthy liver to metabolize it. If ammonia levels rise, confusion and lethargy (encephalopathy) may occur.
- Portal hypertension: An increase in pressure within the liver can cause blood flow issues leading to portal hypertension. This may back up blood flow from other organs, causing splenomegaly, an enlarged spleen, and varices, swollen veins, especially in the esophagus and stomach can predispose to bleeding.
- Osteoporosis: PBC is also complicated by osteoporosis, difficulty in absorbing nutrients, such as fat-soluble vitamin D and calcium, from the intestine.
- Cancer: Some studies show patients with PBC are at an increased risk for hepatocellular carcinoma.
Can primary biliary cirrhosis be prevented?
Since the cause of the disease is not known, it is not possible to prevent PBC. However, medications may be able to slow the progression of the disease and control the symptoms.
Should a person develop PBC, all attempts should be made to prevent further potential damage. This may include limiting alcohol intake and avoiding the use of medications that contain acetaminophen (Tylenol, Panadol), and cholesterol-lowering agents.
Subscribe to MedicineNet's Daily Health News Newsletter
By clicking Submit, I agree to the MedicineNet's Terms & Conditions & Privacy Policy and understand that I may opt out of MedicineNet's subscriptions at any time.
Springer 2010.
Top Primary Biliary Cirrhosis (PBC) Related Articles

Antinuclear Antibody Test
Read about antinuclear antibody tests (ANAs), unusual antibodies that can bind to certain structures within the nucleus of the cells. Antinuclear antibodies are found in patients whose immune system may be predisposed to cause inflammation against their own body tissues. Learn how the ANA test procedure is performed and interpretation of results determined.
Cirrhosis
Cirrhosis of the liver refers to a disease in which normal liver cells are replaced by scar tissue caused by alcohol and viral hepatitis B and C. This disease leads to abnormalities in the liver's ability to handle toxins and blood flow, causing internal bleeding, kidney failure, mental confusion, coma, body fluid accumulation, and frequent infections.Symptoms include yellowing of the skin (jaundice), itching, and fatigue. The prognosis is good for some people with cirrhosis of the liver, and the survival can be up to 12 years; however, the life expectancy is about 6 months to 2 years for people with severe cirrhosis with major complications.

Complete Blood Count (CBC)
A complete blood count (CBC) is a calculation of the cellular makeup of blood. A CBC measures the concentration of white blood cells, red blood cells, platelets in the blood, and aids in diagnosing conditions and disease such as malignancy, anemia, or blood clotting problems.
How Long Can You Live With Cirrhosis?
The life expectancy of people with liver cirrhosis is typically predicted through the following variables.
Itching
Itching can be a common problem. Itches can be localized or generalized. There are many causes of itching including infection (jock itch, vaginal itch), disease (hyperthyroidism, liver or kidney), reactions to drugs, and skin infestations (pubic or body lice). Treatment for itching varies depending on the cause of the itch.
Jaundice in Adults
Jaundice or hyperbilirubinemia in adults is caused by an underlying disease or condition. Learn about when to worry about jaundice in adults, symptoms, treatment, causes, diagnosis, and prevention.
Liver Blood Tests
An initial step in detecting liver damage is a simple blood test to determine the presence of certain liver enzymes in the blood. Under normal circumstances, these enzymes reside within the cells of the liver. But when the liver is injured, these enzymes are spilled into the bloodstream and can lead to diseases like fatty liver, type 2 diabetes, obesity, and hepatitis. Several medications also can increase liver enzyme test results.
Liver Disease Quiz
What is liver disease? Take the Liver Disease Quiz and test your knowledge about this organ and its function.
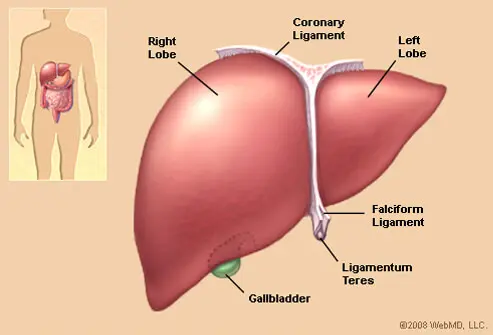
Liver Picture
Front View of the Liver. The liver is a large, meaty organ that sits on the right side of the belly. See a picture of the Liver and learn more about the health topic.
MRI (Magnetic Resonance Imaging Scan)
MRI (or magnetic resonance imaging) scan is a radiology technique which uses magnetism, radio waves, and a computer to produce images of body structures. MRI scanning is painless and does not involve X-ray radiation. Patients with heart pacemakers, metal implants, or metal chips or clips in or around the eyes cannot be scanned with MRI because of the effect of the magnet.
Urinalysis (Urine Test)
Urinalysis (urine test, drug test) is a test performed on a patient's urine sample to diagnose conditions and diseases such as urinary tract infection, kidney infection, kidney stones, and inflammation of the kidneys, or screen for progression of conditions such as diabetes and high blood pressure.
What Are the 4 Stages of Cirrhosis of the Liver?
Stages of cirrhosis of the liver include steatosis, scarring (fibrosis), cirrhosis, and liver failure (hepatic failure).