Common Skin Cancer Symptoms and Causes

Sunlight contains ultraviolet light that is harmful to human skin cells. These energetic light waves can produce mutations in the DNA of skin cells, which in turn can lead to skin cancer. In areas close to the equator, the incidence of cutaneous cancers is dramatically higher due to the increase in sun exposure.
The most obvious skin cancer warning sign is the development of a persistent bump or spot in an area of sun-damaged skin. These spots are likely to bleed with minimal trauma and produce a superficial erosion.
Ultraviolet Light and Skin Cancer
Ultraviolet rays are classified by three types: UVA, UVB, and UVC. UVC is very dangerous, but it does not reach the earth’s surface due to the ozone layer. Exposure to both UVA and UVB radiation poses potential skin cancer risks.
UVA Radiation
UVA light is the most abundant source of solar radiation. Scientists think it can penetrate the top layer of skin, potentially damaging connective tissue and causing skin cancer. An estimated 50% of UVA exposure occurs in the shade. Light skin is far more vulnerable to UVA radiation: while dark skin allows only 17.5% of UVA to penetrate, light skin allows 55% of UVA light to pass through.
UVB Radiation
Sunburns are mostly caused by UVB radiation. Because of the ozone layer, UVB light accounts for only about 5% of the light that reaches the earth’s surface. UVB light can be filtered out by glass windows and does not penetrate as far into the skin as UVA, but it can still cause some forms of skin cancer. UVB is absorbed directly by DNA. Dark skin is twice as effective as light skin at protecting against UVB penetration.
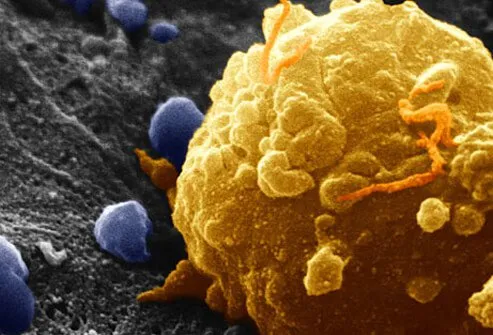
How Skin Cancer Develops
UV light causes skin cancer by damaging the skin’s cellular DNA. That damage is caused by free radicals, which are hyperactive molecules found in UV light. Free radicals cause damage to the DNA double helix, changing the way cells replicate and naturally die, which is how cancer develops. In addition to sun exposure, free radicals are also found in environmental pollutants, cigarette smoke, alcohol, and other toxins.
Skin Cancer: Actinic Keratosis (Solar Keratosis)

Actinic keratoses are scaling, horny, red, tender bumps present in sun-exposed areas. They are essentially very thin skin cancers that have not yet penetrated into deeper tissues. Large areas of skin thus exposed over years can result in what has recently been called a cancerization field defect. Continued exposure to ultraviolet light will likely induce invasive malignancies. Prevention and treatment of this condition which is most common in less-pigmented people is a significant part of medical skin care.
Skin Cancer: Actinic Cheilitis (Farmer's Lip)

Actinic cheilitis is simply actinic keratoses affecting the mucous membranes of the lips (vermillion border). This condition usually involves the lower lip simply because of the angle of incidence at which the overhead light waves hit the face. The forehead, cheeks, nose, and lower lip receive light waves perpendicularly and are not shaded by anatomical structures like the brows.
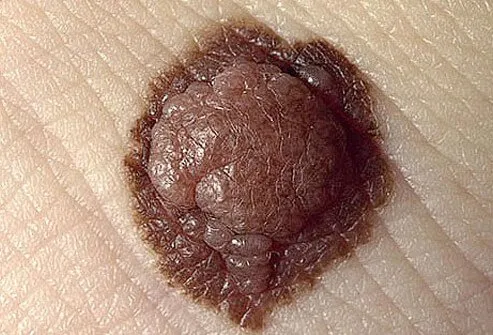
Skin Cancer: Cutaneous Horns

A cutaneous horn is a mass of dead skin cells. Essentially they have a lot in common with hair and nails since these are also composed of dead skin cells. The base which generates the horn can be an actinic keratosis, a squamous cell carcinoma, or a benign keratosis. The only way to differentiate between the three is by performing a surgical procedure called a biopsy and having it examined in a laboratory by a pathologist.
Identifying Cancerous Moles
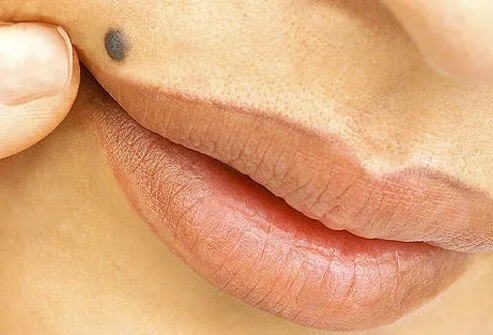
The word "mole" is probably derived from a German word meaning spot. In the context of skin, a mole is a long-lasting skin spot that is a little darker than a freckle. Since there are a variety of benign and malignant skin growths which fulfill this description, more precision is necessary. The number of moles present on a particular person is most closely related to skin color and the extent of exposure to sunlight during childhood. The average number of moles is about 35 per person in Northern European populations.
Melanocytic Nevus
Moles that are melanocytic nevi (nevus singular) are local growths of melanocytes which can be present at birth or may develop after birth well into the third decade. They vary in color from black to flesh-colored. A melanocytic nevus can develop into melanoma, particularly if the nevus is large. The risk of a congenital melanocytic nevus developing into melanoma is greater for children under 10, which account for 70% of all cases.
Atypical Moles

When a physician examines a particular spot or mole it can appear either ordinary or peculiar. Most of these atypical nevi -- when examined under the microscope -- are not cancer; it seems to be the new lesions that develop in adulthood that are the ones that are most likely to be malignant melanomas.
The term dysplastic refers to changes noted in moles that can only be appreciated on microscopic examination. This term should only be used when describing the microscopic appearance of a nevus or other tissue. Most atypical nevi exhibit some degree of dysplasia under the microscope.
ABCDEs of Melanoma

In an attempt to systemize nevus description, physicians use a variety of adjectives to describe visible alterations. To simplify things, benign lesions are almost always uniform in color, circular in shape, and exhibit bilateral symmetry about any axis drawn through its diameter. Malignant melanomas diverge from this appearance to a greater or lesser extent. To help one remember the criteria, they have been called the ABCDEs (mnemonic – stands for asymmetry, border, color, diameter and evolving) of nevus description. Another valuable consideration is the so-called "ugly duckling" nevus which appears significantly different than all the other skin spots on the patient
Melanoma Symptoms: 'A' Is for Asymmetry

Asymmetry refers to the degree of similarity when one compares the appearance of each of four quadrants produced by an imaginary cross through the middle of a melanocytic nevus.
Melanoma Symptoms: 'B' Is for Border

Border refers to degree of circular regularity of the edge of a pigmented lesion. Perfectly circular lesions are rarely malignant.
Melanoma Symptoms: 'C' Is for Color

Color: The degree of uniformity of color is a measure of atypicality. The more colors present the more likely the lesion is to be malignant.
Melanoma Symptoms: 'D' Is for Diameter
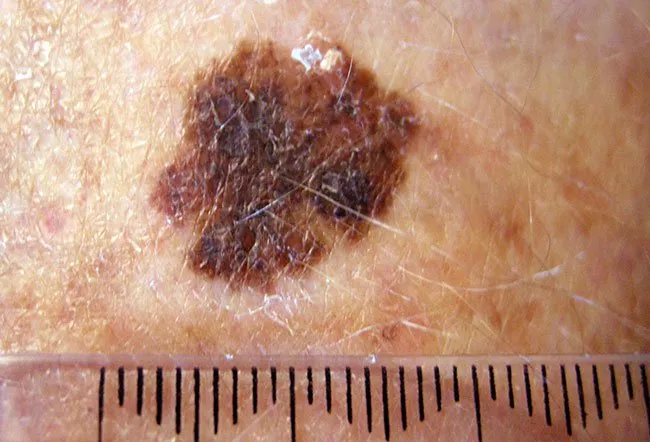
Diameter: Although malignant pigmented lesions tend to be larger than a pencil eraser this is one of the less reliable criteria for distinguishing melanomas.
Melanoma Symptoms: 'E' Is for Evolving
Evolving: Malignancies by their very nature tend to change over time -- mostly by increasing in size -- as opposed to benign lesions that are stable. Since cancers grow in an uncontrolled way, they tend to produce asymmetrical lesions.
Screening for Cancerous Moles

If a mole looks or acts at all peculiarly it is best to have it evaluated by an expert. This frequently is a dermatologist. Most dermatologists can tell if the pigmented lesion is composed of melanocytes or is something quite different with no possibility of being a melanoma. Many dermatologists now use a hand-held magnifying device which produces polarized light to evaluate colored melanocytic tumors. The use of this instrument improves the doctor's ability to identify suspicious lesions.
Evaluating Potentially Cancerous Moles

The decision on which mole needs to be examined depends on the concern the doctor has that it may be cancerous. Since the procedure necessary to take off the suspicious bump is simple, requiring only local anesthesia and rarely is associated with complications, the threshold for this procedure is appropriately low. If the lesion is melanocytic in origin and it appears at all peculiar, exhibiting any of the features addressed in the ABCDE criteria and/or the patient complains that the bump bleeds or is irritated or itchy, that is often enough to trigger a biopsy.
Malignant Melanoma
Malignant melanoma is the most deadly form of skin cancer because it tends to spread at a very early stage to other parts of the body. The likelihood that it has spread is most directly related to the thickness of the melanoma as measured from its surface to its depth by a pathologist. This information is communicated to the doctor that submitted the nevus and subsequent treatment depends on this information.
Melanoma Symptoms
In addition to the ABCDEs of melanoma, there are other melanoma symptoms that may include:
- A sore that will not heal
- Pigment that spreads from the border of a spot into the surrounding skin
- Redness or swelling around a skin spot
- A spot that becomes itchy, tender, or painful
- Scaliness, bleeding, or oozing from the surface of a mole
How Melanoma Cancer Develops

Although it is possible for a previously benign mole to become malignant, most of the time a melanoma cancer begins as a single malignant cell in previously normal skin and then continues to grow in an uncontrolled manner.
Squamous Cell Carcinoma

Squamous cell carcinomas begin as malignancies of living epidermal cells which grow and invade into the deeper layers of the skin. They usually begin as an actinic keratosis and progress over many years. Although most actinic keratoses do not eventuate into squamous cell cancers, if one has a great many of them and they continue to receive sufficient ultraviolet irradiation producing sufficient mutational events, it is extremely likely that a squamous cell carcinoma will develop. They appear as thick, keratotic bumps on sun-exposed skin which continue to enlarge. They do not commonly spread to distant sites, but larger lesions can do this.
Bowen Disease: Is it Cancer?

So called "Bowen's disease" lesions are simply squamous cell carcinomas that have not as yet penetrated into the deeper layers of the skin. They involve the entire thickness of the most superficial living layer of the epidermis as opposed to actinic keratoses which involve the upper half of the epidermis. They seem to be a stage in the progression of an actinic keratosis to an invasive squamous cell carcinoma. As such it is cancer. Bowen disease is easily curable by cryotherapy, curettage with cautery and other methods.
Basal Cell Carcinoma

Basal cell carcinomas arise from the layer of skin cells present along the lowest layer of the epidermis and are the most common form of skin cancer. They are locally aggressive so they ought to be treated before they get so large that removal becomes difficult. The tumor has a shiny surface, is pearly white in color, and tends to bleed quite easily. It often ulcerates.
Who Is At Risk for Skin Cancer and Why?

Sunlight is by far the most common cause of skin cancer. Most of the exposure occurs during leisure time or sun tanning. The perceived benefits of exposure to sunlight seem to be confined mostly to the production of vitamin D in the skin and a belief that darker skin is more aesthetically appealing. Vitamin D requirements can be easily satisfied with dietary supplementation. Light-skinned individuals with blonde or red hair who live in regions near the equator are the most at risk to develop skin cancer.
Reduce Your Skin Cancer Risk

Beyond living a healthy lifestyle, it is important to avoid exposure to sunlight as much as is reasonably possible. Eating a balanced diet and staying physically active improves the body’s ability to fight free radical damage and heal.
Protecting Your Skin
Any time there has been a darkening of the skin after sun exposure it is a sign that some damage has been sustained. Since the incubation period for skin cancers and photo-aging is quite long (5 to 15 years), it may be difficult to convince sun worshipers to head indoors.
Avoiding UV Damage
The use of clothing, searching for shade, and the application of effective, broad-spectrum sunscreens are all useful behaviors in limiting sun damage.
Seeking Shade to Avoid Skin Cancer
Shade is the first defense against skin damage. Between the hours of 10 a.m. and 4 p.m., when the sun’s rays are at their most intense, find cover or wear a wide-brimmed hat. The Skin Cancer Foundation recommends hats with broad brims all around that are at least three inches wide.
Although shade is an important protection against skin cancer, it may still leave you vulnerable to UVB light, which can reach skin indirectly. UV radiation can bounce off of clouds, dry sand, concrete and other UV-reflective surfaces.
Choosing the Right Sunscreen
Sunscreens that are reasonably durable are currently available that block all the wavelengths of ultraviolet light with an SPF (Sun Protection Factor) of 50. It can help to look for the words “broad spectrum” or “multi spectrum” when choosing a sunscreen. This indicates that both UVA light and UVB light are being blocked by your sunscreen. Keep in mind that these phrases don’t actually indicated how much of each ray is being blocked. Also, consider using an FDA approved “Water Resistant (40 or 80 min.)” sunscreen if you sweat or swim in sunlight.
Additional Information on Skin Cancer
For more information about Skin Cancer, please consider the following:
Skin Cancer Symptoms, Types, Images
This tool does not provide medical advice. See additional information: 
© 1996-2024 WebMD, LLC. All rights reserved.