What is a subconjunctival hemorrhage?

The conjunctiva is the clear tissue that covers the white of the eye (the sclera) and lines the inside of both eyelids. A subconjunctival hemorrhage is blood from a tiny broken blood vessel located between the conjunctiva and the underlying sclera.
What usually causes a subconjunctival hemorrhage?
The conjunctiva contains nerves and many small blood vessels. These blood vessels are usually barely visible but become larger and more visible if the eye is inflamed. These blood vessels are somewhat fragile and their walls break easily, resulting in a subconjunctival hemorrhage (bleeding under the conjunctiva).
A subconjunctival hemorrhage appears as a bright red or dark red patch on the sclera. Most subconjunctival hemorrhages are spontaneous without an obvious cause for the bleeding. They come from normal conjunctival blood vessels. Since most subconjunctival hemorrhages are painless, a person may discover a subconjunctival hemorrhage only by looking in the mirror. Many spontaneous subconjunctival hemorrhages are first noticed by another person seeing a red spot on the white of your eye.
Rarely there may be an abnormally large or angulated blood vessel as the source of the hemorrhage.
The following can occasionally result in a spontaneous subconjunctival hemorrhage:
- Sneezing
- Coughing
- Straining/vomiting or a Valsalva maneuver, increasing the pressure in the veins of the head, as in weight lifting or lying on an inversion table upside-down
- Eye rubbing or inserting contact lenses
- Certain infections of the outside of the eye (conjunctivitis) where a virus or a bacteria weaken the walls of small blood vessels under the conjunctiva
- A medical disorder causing bleeding or inhibiting normal clotting
- The use of anticoagulant medication such as warfarin (Coumadin, Jantoven) or other blood thinners
Subconjunctival hemorrhage can also be non-spontaneous and result from hemorrhagic conjunctivitis, a severe eye infection, trauma to the head or eye, or after cataract surgery, other eye surgery, or eyelid surgery.
What are the risk factors for subconjunctival hemorrhage?
Most subconjunctival hemorrhages are spontaneous and not linked to any specific risk factors.
If the hemorrhage is not spontaneous, then the risk factors for subconjunctival hemorrhage include the following:
- Trauma to the eye
- Eye surgery
- The use of contact lenses
- The use of medication that inhibits clotting or promotes bleeding
- Diseases that are characterized by decreases in platelet count or vascular fragility
Because of the association between increasing vascular fragility and advanced age, being older also includes an increased risk of subconjunctival hemorrhage.
What are symptoms of a subconjunctival hemorrhage?
Most of the time, no symptoms are associated with a subconjunctival hemorrhage other than seeing blood over the white part of the eye or "blood in the whites of the eye." The hemorrhage does not extend over your pupil therefore your vision is not affected.
- Very rarely do people experience pain when the hemorrhage begins. When the bleeding first occurs, one may notice a sense of fullness in the eye or under the lid. Mild pressure around the eye may also be experienced. There is no associated headache. As the hemorrhage resolves, some people may feel very mild irritation of the eye or merely a sense of awareness of the eye.
- The hemorrhage itself is a prominent, sharply outlined bright red area overlying the sclera. The entire white part of the eye may occasionally be covered by blood.
- In a spontaneous subconjunctival hemorrhage, no blood will exit from the eye. If one blots the eye with a tissue, there should be no blood on the tissue.
- The hemorrhage will appear larger within the first 24 hours after its onset and then will slowly decrease in size as the blood is absorbed.
Should I go to urgent care for a subconjunctival hemorrhage?
Call a primary care provider or ophthalmologist (a medical doctor specializing in eye care and surgery) if the subconjunctival hemorrhage does not get better within two weeks or if it has happened multiple times.
Also, call your healthcare provider if you have a hemorrhage in both eyes simultaneously or if the subconjunctival hemorrhage coincides with a new onset of easy bruising or bleeding gums.
When should I be concerned about a subconjunctival hemorrhage?
Go to a doctor immediately if the subconjunctival hemorrhage is associated with the following:
- Pain
- Changes in vision (for example, blurry vision, double vision, difficulty seeing)
- A history of recent injury or trauma
- A history of bleeding disorder
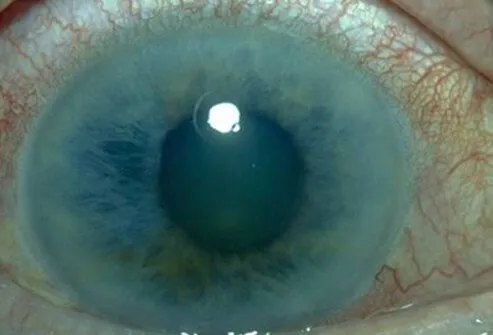
IMAGES
Subconjunctival Hemorrhage See a picture of eye diseases and conditions See ImagesWhat specialists diagnose and treat a subconjunctival hemorrhage?
Your primary care provider or ophthalmologist can make the diagnosis. That physician can also order tests if you have a recent history of easy bruising.
How do healthcare professionals diagnose a subconjunctival hemorrhage?
A healthcare provider will take a medical history and medication history to determine what events were leading up to the subconjunctival hemorrhage and will also perform an examination. Vital signs including blood pressure may also be checked.
- If the trauma was the cause, a more thorough examination will usually be performed.
- In newborn infants, subconjunctival hemorrhage can occasionally be found as a result of the birth process.
How do you treat a subconjunctival hemorrhage?
Usually, no treatment is needed. Over-the-counter artificial tears can be applied to the eye if mild irritation is present. The eye does not require a patch.
The use of aspirin or other medication that inhibits clotting should be avoided. If you are taking aspirin or an anticoagulant for a medical condition, check with your physician to determine whether the medication should be stopped or continued. Do not stop anti-coagulation medicines without physician consultation. These medications are frequently lifesavers, and they rarely need to be discontinued for a subconjunctival hemorrhage.
- If the subconjunctival hemorrhage is trauma-related, an ophthalmologist will determine what other treatment is necessary to promote the healing of the injury.
- If the subconjunctival hemorrhage is a result of external infection, an ophthalmologist may prescribe antibiotic drops or an ointment.
This condition clears by itself within one to two weeks. Recovery is usually complete, without any long-term problems, similar to a mild bruise under the skin. Like a bruise, a subconjunctival hemorrhage changes colors (often red to orange to yellow) as it heals. A skin bruise changes to various shades of green, black, and blue as it heals, because the blood is being seen through the skin. Because the conjunctiva is transparent, a subconjunctival hemorrhage never has these color characteristics.
Very rarely, with recurrent subconjunctival hemorrhage in the same location in the same eye, there may be an abnormal fragile capillary within the conjunctiva that has thin walls and tends to bleed spontaneously. An ophthalmologist can identify such a condition and close this non-essential blood vessel using heat, either from a laser or a diathermy unit.
Health News
- More of America's Pets Are Overdosing on Stray Coke, Meth
- GLP-1 Zepbound Is Approved As First Drug For Sleep Apnea
- Feeling Appreciated by Partner is Critical for Caregiver's Mental Health
- Tips for Spending Holiday Time With Family Members Who Live with Dementia
- The Most Therapeutic Kind of Me-Time
 More Health News »
More Health News »
Are there home remedies for a subconjunctival hemorrhage?
Because of the benign nature of most subconjunctival hemorrhages, there is no need for home remedies.
What is the prognosis for subconjunctival hemorrhage?
The prognosis of subconjunctival hemorrhage is excellent when it occurs in the absence of trauma. It will spontaneously become smaller and disappear in less than two weeks. It will cause no scarring visual loss or other ocular changes.
What are possible complications of a subconjunctival hemorrhage?
A subconjunctival hemorrhage will not cause any complications unless it is associated with trauma to the eye or a recent history of easy bruising.
Is it possible to prevent a subconjunctival hemorrhage?
If you are having frequent subconjunctival hemorrhages or your subconjunctival hemorrhage is associated with easy bruising or bleeding elsewhere, you should have a medical evaluation for an underlying bleeding or clotting problem. Successful treatment of such an underlying condition may prevent future hemorrhages.
Top Subconjunctival Hemorrhage Related Articles

Blood Disorders Quiz
Exactly what is sickle cell anemia? Learn about sickle cell and other diseases by testing your IQ with the Blood and Bleeding Disorders Quiz.
Brain Hemorrhage
A brain hemorrhage is a type of stroke caused when an artery bursts in the brain, causing localized bleeding in the surrounding tissue. Causes of brain hemorrhage include aneurysm, liver disease, brain tumor, head trauma, high blood pressure, and blood vessel abnormalities. Symptoms and signs include sudden severe headache, nausea, vomiting, loss of balance, tingling, numbness, vision changes, loss of consciousness, and loss of fine motor skills. Treatment depends upon the cause, location, and size of the brain hemorrhage.
Chronic Cough
Chronic cough is a cough that does not go away and is generally a symptom of another disorder such as asthma, allergic rhinitis, sinus infection, cigarette smoking, GERD, postnasal drip, bronchitis, pneumonia, medications, and less frequently tumors or other lung disease.Chronic cough treatment is based on the cause, but may be soothed natural and home remedies.

Eye Care
Many common eye disorders resolve without treatment and some may be managed with over-the-counter (OTC) products. It's important to visit a physician or ophthalmologist is the problem involves the eyeball itself or the condition hasn't improved after 72 hours of use of an OTC eye care product.
Common Eye Problems
Eye diseases can cause damage and blindness if not treated soon enough. Learn the warning signs and symptoms of common eye conditions such as glaucoma, cataracts, pink eye, macular degeneration and more.
Eye Picture
The eye has a number of components which include but are not limited to the cornea, iris, pupil, lens, retina, macula, optic nerve, choroid and vitreous. See a picture of the Eye and learn more about the health topic.
Eye Conditions Quiz
What do you know about your eyes? Take this quick quiz to learn about a range of eye diseases and conditions.
Nausea and Vomiting
Nausea and vomiting are symptoms of many conditions including motion sickness, pregnancy, emotional stress, gallbladder disease, and other illnesses. Learn about causes, treatment, and when to be concerned.
Over-the-Counter Products
OTC drugs are available without a prescription, simply "over the counter." Find an easy-to-follow format to help you understand which products may work better for specific conditions and how to choose the products that are most appropriate.
Pinkeye
Pinkeye, also called conjunctivitis, is redness or irritation of the conjunctivae, the membranes on the inner part of the eyelids, and the membranes covering the whites of the eyes. These membranes react to a wide range of bacteria, viruses, allergy-provoking agents, irritants, and toxic agents.
plasma protein fraction
Plasma protein fraction is a blood product used for the treatment of shock and low blood volume (hypovolemia) from plasma fluid loss due to burns, crushing injuries, abdominal emergencies, or any other cause where there is a significant loss of plasma fluids and not red blood cells. It is also used as an emergency treatment of shock due to hemorrhage, which may be followed by blood transfusion if required. Common side effects of plasma protein fraction include nausea, vomiting, excessive salivation, headache, back pain, chills, fever, redness of skin (erythema), hives (urticaria), severe allergic reaction (anaphylaxis), flushing, fluid in lungs (pulmonary edema), shortness of breath (dyspnea), low blood pressure (hypotension), and rapid heart rate (tachycardia).
Shaken Baby Syndrome (Abusive Head Trauma)
Shaken baby syndrome, or abusive head trauma, is the condition that describes the symptoms and signs that result from the violent shaking of an infant. These symptoms and signs include bruising, vomiting, poor feeding, seizures, head trauma, and hemorrhages of the retina. Shaken baby syndrome treatment involves removing the infant from the household where the abuse occurred and providing supportive care for the child's injuries.