- Things to Know
- Types
- Causes
- Risk Factors
- Signs & Symptoms
- Incubation & Contagious Period
- Diagnosis
- Treatment Chart
- Doctor Specialists
- Complications
- Prognosis
- Prevention
-
Comments
-
**COMMENTSTAGLIST**
-
More
-
**OTHERTAGLIST**
Things to know about tuberculosis (TB)
- Tuberculosis (TB) is an infectious disease that's transmitted from person to person.
- Consumption: an old and once common term for wasting away of the body, particularly from pulmonary tuberculosis (TB) at certain times in the past used interchangeably with TB
- There are many different types of TB.
- A bacterium, Mycobacterium tuberculosis, causes the disease.
- There are many risk factors for TB. Clinical symptoms and signs of pulmonary TB include fever, night sweats, cough, hemoptysis (coughing up blood-stained sputum), weight loss, fatigue, and chest pain.
- TB is contagious; the incubation and contagious periods may vary.
- Physicians definitively diagnose TB by culturing mycobacteria from sputum or biopsy specimens, but healthcare professionals presumptively diagnose TB by history, physical exam, skin testing, and chest X-rays.
- Treatment of TB infection is related to the type of TB infection and often requires extended treatments (months) with one or more anti-TB drugs.
- Complications of TB range from none to chronic problems and death and include lung, kidney, and liver problems that can be severe.
- The prognosis for appropriately treated TB infection is good. The prognosis declines in people who develop complications or who have had previous TB treatments.
- Prevention of TB involves both early treatments to reduce transmission and isolation of the infected person until they are no longer contagious. There is a vaccine against TB, but it is not used routinely in the U.S. because of efficacy issues and other problems.
What is tuberculosis?
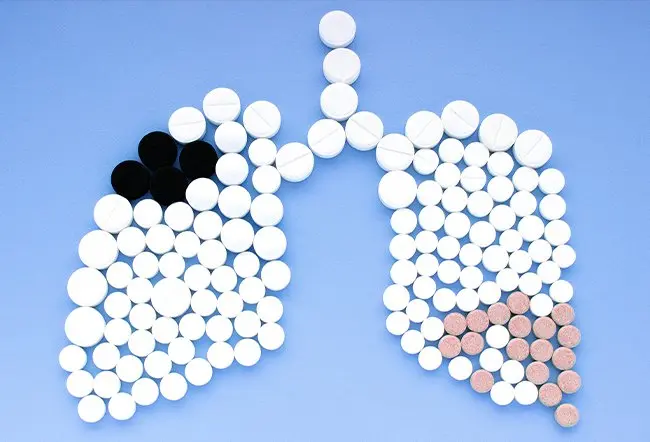
Tuberculosis (TB) is a multisystemic infectious disease caused by Mycobacterium tuberculosis (or TB, TB germs), a rod-shaped bacterium. TB (TB may stand for the disease or the bacteria that cause the disease) is the most common cause of infectious disease-related mortality worldwide (about 10 million people worldwide were sick with TB in 2017, and about 1.3 million people died from TB worldwide in 2017 according to the World Health Organization [WHO] and the CDC). HIV-associated TB infections are a leading cause of death in HIV patients. TB symptoms can span such a wide range that TB is termed the "great imitator" by many who study infectious diseases because TB symptoms can mimic many other diseases. Additional terms describe TB. The terms include consumption, Pott's disease, active, latent, pulmonary, cutaneous, and others (see the following section), and they appear in both medical and nonmedical publications. In most instances, the different terms refer to a specific type of TB with some unique symptoms or findings. The most common site (about 85%) for TB to develop is in the pulmonary tract although it may infect other parts of the body. Humans are the only known hosts for Mycobacterium tuberculosis (although it can infect animals). The bacteria may stain weakly both gram-negative and gram-positive due to their cell surface so medical professionals use acid-fast stains to visualize the cells with a microscope.
TB has likely been infecting humans for many centuries; evidence of TB infections has been found in cadavers that date back to about 8000 BC. The Greeks termed it wasting away disease (phthisis). For many European countries, TB caused death in about 25% of adults and was the leading cause of death in the U.S. until the early 1900s. Robert Koch discovered TB's cause, Mycobacterium tuberculosis, in 1882. With increased understanding of TB, public health initiatives, treatment methods like isolation of patients (quarantine), and the development of drugs to treat TB, the incidence of the disease, especially in developed countries, has been markedly reduced. However, the CDC estimates one-third of the world's population is infected with TB with about 1.8 million deaths per year. About 60% of all TB-infected people are located in India, Indonesia, China, Nigeria, Pakistan, and South Africa.
There is a vast amount of detailed information available in the medical literature on all aspects of this potentially debilitating and lethal disease. The goal of this article is to introduce the reader to TB and help them to obtain general knowledge about TB's cause, transmission, diagnostic tests, treatments, and prevention methods against tuberculosis infection.

SLIDESHOW
Bacterial Infections 101: Types, Symptoms, and Treatments See SlideshowAre there different types of tuberculosis (TB)?
There are many types of tuberculosis, but the main two types are termed either active or latent tuberculosis infection. Active TB is when the disease is actively producing symptoms and can be transmitted to other people; latent disease is when the person is infected with Mycobacterium tuberculosis bacteria, but the bacteria are not producing symptoms (usually due to the body's immune system suppressing the bacterial growth and spread) and have no TB bacteria in the sputum. People with latent TB usually cannot transfer Mycobacterium tuberculosis bacteria to others unless the immune system fails; the failure causes reactivation (bacterial growth is no longer suppressed) that results in active TB so the person becomes contagious. Latent TB resembles a chickenpox infection that goes dormant and may reactivate years later.
Many other types of TB exist in either the active or latent form. These types are named for the signs and the body systems Mycobacterium tuberculosis preferentially infect, and these infection types vary from person to person. Consequently, pulmonary tuberculosis mainly infects the pulmonary system (lungs), cutaneous TB has skin symptoms, while miliary TB describes widespread small infected sites (lesions or granulomas about 1 mm-5 mm) found throughout body organs. It is not uncommon for some people to develop more than one type of active TB. More types will be listed in the symptoms and signs section below.
Atypical mycobacteria that may cause disease are the M. avium complex, M. fortuitum complex, and M. kansasii.
Health News
- More of America's Pets Are Overdosing on Stray Coke, Meth
- GLP-1 Zepbound Is Approved As First Drug For Sleep Apnea
- Feeling Appreciated by Partner is Critical for Caregiver's Mental Health
- Tips for Spending Holiday Time With Family Members Who Live with Dementia
- The Most Therapeutic Kind of Me-Time
 More Health News »
More Health News »
What causes tuberculosis?
The cause of TB is an infection of human tissue(s) by the bacterium Mycobacterium tuberculosis (mycobacteria or TB). These bacteria are slow-growing, aerobic, and can grow within body cells (an intracellular parasitic bacterium). Its unique cell wall helps protect it from the body's defenses and gives mycobacteria the ability to retain certain dyes like fuchsin (a reddish dye) after an acid rinse that rarely happens with other bacterial, fungal, or parasitic genera.
Mycobacteria that escape destruction by body defenses may be spread by blood or lymphatic pathways to most organs, with a preference for those that oxygenate well (lungs, kidneys, and bones, for example). Typical TB lesions, termed granulomas, usually consist of a central necrotic area, then a zone with macrophages, giant Langerhans cells, and lymphocytes that become surrounded by immature macrophages, plasma cells, and more lymphocytes. These granulomas also contain mycobacteria. In latent infections, a fibrous capsule usually surrounds the granulomas, and in some people, the granulomas calcify, but if the immune defenses fail initially or at a later time (reactivate), the bacteria continue to spread and disrupt organ functions.
What are risk factors for tuberculosis?
Although TB is not easily spread, it is usually spread between people who are in close contact (working together or living together).
There are many risk factors for developing tuberculosis. Certain groups of people have a high risk, such as people who work in hospitals and other areas where TB-infected people may reside (jails, nursing homes, group homes for HIV patients, homeless shelters). Close association with drug users or people with known TB infections are also at higher risk.
Other people at high risk include the following:
- Visitors and immigrants from areas known to have a high incidence of TB
- Children and the elderly with weakened immune systems (especially those with a positive TB skin test, see below)
- Patients with HIV infection
- Drug abusers, especially IV drug abuse
- Head and neck cancer patients
- Transplant patients
- Diabetics
- Kidney disease patients
- People undergoing immunosuppressive therapy
- Silicosis
Subscribe to MedicineNet's Daily Health News Newsletter
By clicking Submit, I agree to the MedicineNet's Terms & Conditions & Privacy Policy and understand that I may opt out of MedicineNet's subscriptions at any time.
What are tuberculosis symptoms and signs?
Although there are several TB types, pulmonary tuberculosis is responsible for the majority (about 85%) of TB infections. Consequently, pulmonary TB symptoms and signs may occur with or even before other types of TB are diagnosed.
The classical clinical symptoms and signs of pulmonary TB may include the following:
- Fever
- Night sweats
- Cough (often chronic)
- Hemoptysis (coughing up bloody sputum)
- Decrease or loss of appetite
- Weight loss and/or muscle loss (unintentional)
- Fatigue and/or malaise
- Chest pain (pain while breathing)
- Shortness of breath
- Swollen lymph nodes
- Pneumonitis (maybe the only symptom in the elderly).
Other types are loosely classified as extrapulmonary and often have symptoms that are nonspecific but frequently localized to the involved site.
The following includes the signs and symptoms of additional types of TB:
- Skeletal TB (also termed Pott's disease): spinal pain, back stiffness, and paralysis is possible
- TB meningitis: headaches (variable in length but persistent), mental changes, coma
- TB arthritis: usually pain in a single joint (hips and knees most common)
- Genitourinary TB: dysuria, flank pain, increased frequency, masses or lumps (granulomas)
- Gastrointestinal TB: difficulty swallowing, nonhealing ulcers, abdominal pain, malabsorption, diarrhea (may be bloody)
- Miliary TB: many small nodules widespread in organs that resemble millet seeds (hence its name)
- Pleural TB: empyema and pleural effusions
- Multidrug-resistant tuberculosis (MDR TB): patients infected with TB bacteria that are resistant to multiple drugs
- XDR TB: patients infected with TB bacteria that are resistant to some of the most effective anti-TB medications; XDR stands for extensively drug-resistant
- Caseous TB: Necrotic (dead and dying) tissue that is infected with TB organisms has a soft, dry, and cheesy appearance.
- End-stage TB: Patients may suffer fever, constant coughing, shortness of breath, weight loss, mental changes, and blood in their sputum before death.
From 
Infectious Disease Resources
Is TB contagious, and how long is the incubation period and contagious period?
TB is contagious and can be spread to others by airborne droplets during sneezing, coughing, and contact with sputum, so you can get the disease by close contact with infected people; outbreaks occur in crowded conditions. The incubation period may vary from about two to 12 weeks. A person may remain contagious for a long time (as long as viable TB bacteria are present in the sputum) and can remain contagious until they have been on appropriate therapy for several weeks. However, some people may be infected but suppress the infection and develop symptoms years later; some never develop symptoms or become contagious.
How do physicians diagnose tuberculosis? What is involved with TB testing?
Because TB may occur as either a latent or active form, the definitive diagnosis of active tuberculosis depends on the culture of mycobacteria from sputum or tissue biopsy. However, it may take weeks for these slow-growing bacteria to grow on specialized media. Since patients with latent TB do not require isolation or immediate drug therapy, it is useful to determine if a person is either not infected, has a latent infection, or is actively infected with transmissible TB bacteria. Consequently, doctors needed a presumptive test(s) that could reasonably assure that the person was infected or not so therapy could begin. After getting a patient's history and physical exam data, the next usual test is the skin test (termed the Mantoux tuberculin skin test or the tuberculin skin test or TST, sometimes referred to as a PPD test). The test involves injecting tuberculin (an extract made from killed mycobacteria) into the skin. In about 48-72 hours, the skin is examined for induration (swelling) by a qualified person; a positive test (induration) strongly suggests the patient has either been exposed to live mycobacteria or is actively infected (or had been vaccinated); no induration suggests the person tests negative for TB. This test can have false-positive results (especially in individuals vaccinated for TB with the BCG vaccine). False-negative results can be caused by patients who are immunocompromised.
Another test, IGRA (interferon-gamma release assays) can measure the immune response to Mycobacterium tuberculosis. Other quick tests are useful; chest X-rays can give evidence of lung infection while a sputum smear stained with certain dyes that are retained mainly (but not exclusively) by mycobacteria can show the presence of the bacterium. These tests, when examined by a doctor, are useful in establishing a presumptive diagnosis of either latent or active TB, and most doctors will initiate treatment based on their judgment of these tests. In addition, some of these tests are useful in the U.S. and elsewhere only in people who are not vaccinated with a TB vaccine (see below) but are less useful in vaccinated people. For some patients, culture studies still should be completed to determine the drug susceptibility of an infecting TB strain.
Other tests have been developed. For example, a PCR test (polymerase chain reaction) to detect TB antigens and the LED-FM microscopic technique to identify TB organisms with microscopy may be used. Two other TB blood tests (also called interferon-gamma release assays or IGRAs) have been approved by the FDA and measure how strongly the body's immune system reacts to TB bacteria. IGRAs are recommended in testing patients who have been vaccinated against TB (see prevention section below).
People with positive symptoms, positive blood tests, sputum smear, or culture-positive are considered infected with TB and contagious (active TB).
Physicians diagnose and treat people with latent TB infections (LTBI) according to the following current CDC criteria:
- No symptoms or physical findings suggestive of TB disease
- TST or IGRA result is usually positive
- A chest radiograph is typically normal
- If done, respiratory specimens are smeared and culture-negative
- Cannot spread TB bacteria to others
- Should consider treatment for LTBI to prevent TB disease (strongly advised by the CDC)
What is the treatment for tuberculosis?
The treatment for TB depends on the type of TB infection and drug sensitivity of the mycobacteria. For latent TB, three anti-TB drugs are used in four different recommended schedules. The drugs are isoniazid (INH), rifampin (RIF; Rifadin), and rifapentine (RPT; Priftin) and the CDC's four recommended schedules are below and are chosen by the treating doctor based on the patient's overall health and type of TB the patient was likely exposed to.
| Drugs | Duration | Interval | Minimum Doses |
|---|---|---|---|
| Table reproduced and modified from the CDC; http://www.cdc.gov/tb/topic/treatment/default.htm | |||
| Isoniazid | 9 months | Daily Twice weekly |
270 76 |
| Isoniazid | 6 months | Daily Twice weekly |
180 52 |
| Isoniazid and Rifapentine | 3 months | Once weekly | 12 |
| Rifampin | 4 months | Daily | 120 |
First-line drugs used to treat active TB are INH, RIF, ethambutol (EMB; Myambutol), and pyrazinamide. The CDC offers a guide for the basic treatment schedules for active TB (drug-susceptible TB organisms) as follows:
| Preferred Regimen | Alternative Regimen | Alternative Regimen | |
|---|---|---|---|
| *EMB can be discontinued if drug susceptibility studies demonstrate susceptibility to first-line drugs; Table reproduced and modified from http://www.cdc.gov/tb/topic/treatment/tbdisease.htm#2 | |||
| Initial Phase Daily INH, RIF, PZA, and EMB* for 56 doses (8 weeks) |
Initial Phase Daily INH, RIF, PZA, and EMB* for 14 doses (2 weeks), then twice weekly for 12 doses (6 weeks) |
Initial Phase Thrice-weekly INH, RIF, PZA, and EMB* for 24 doses (8 weeks) |
|
| Continuation Phase Daily INH and RIF for 126 doses (18 weeks) or twice-weekly INH and RIF for 36 doses (18 weeks) |
Continuation Phase Twice-weekly INH and RIF for 36 doses (18 weeks) |
Continuation Phase Thrice-weekly INH and RIF for 54 doses (18 weeks) |
|
The most current treatment guidelines need to be reviewed and correlated to the patient's specific condition and circumstances before any treatment are started.
Treatment of drug-resistant (or antibiotic-resistant) and multi-drug-resistant tuberculosis TB can be difficult. These TB patients may require second-line drugs. Patients with these infections are recommended by the CDC to involve infectious-disease specialists as multiple approaches involve other anti-TB drugs and variable treatment schedules that can be used. In addition, new drugs and treatment schedules are being developed and approved by the FDA. The infectious-disease consultant may be aware of these newest treatments that may benefit specific patients. For example, bedaquiline (Sirturo) has been approved for the treatment of MDR TB, and research with an antimicrobial drug, moxifloxacin, suggests it may help in treatment protocols.
Some side effects of treatment may include the following:
- Loss of appetite
- Nausea and/or vomiting
- Jaundice
- Paresthesia
- Bruise formation, bleeding
- Vision changes
Patients are urged to see their doctor if any side effects occur.
In some patients, the lung destruction may be severe and the only treatment left may be surgical resection of the diseased lung tissue.
Medications are needed for TB treatment. Home remedies will not treat TB but at best may help reduce symptoms. Home remedies may include milk, pineapple, Indian gooseberry, bananas, and many others. Patients should discuss these remedies with their doctors before use.
What types of doctors treat TB?
Although the patient's primary care doctor can oversee and coordinate treatment, other specialists like an infectious disease, pulmonary medicine, internal medicine, critical care, and public health physicians can also be involved in the treatment.
What are complications of tuberculosis?
Although some people may develop no complications, others range from mild to severe complications, including death. Some of the more severe complications include lung function damage, bone pain (spine, ribs, and joints), meningitis, kidney and/or liver malfunction, cardiac tamponade, and visual disturbances.
What is the prognosis of tuberculosis?
For most people who live in areas where diagnosis and treatment are available, the prognosis of TB is good if they complete the treatment protocols. The recurrence rate of TB is low (0%-14%) and some may be due to reinfection. Drug-resistant tuberculosis is more difficult to treat, and the prognosis is not as good. The same poor prognosis occurs for those patients who are immunocompromised (for example, HIV-positive individuals), the elderly, and patients with previous infection and treatment for TB.
How can people prevent tuberculosis?
A vaccine against TB is commercially available; it is termed BCG or Bacille Calmette-Guerin vaccine. However, the vaccine is not recommended for use in the U.S. because of the low risk for TB infections. Also, the vaccine is highly variable in its ability to prevent adult pulmonary disease. Another problem is that the vaccine may interfere with the interpretation of the tuberculin skin test. Despite this, several countries still use it to reduce childhood infections and miliary disease. Consequently, the CDC makes this recommendation: "The BCG vaccine should be considered only for very select persons who meet specific criteria and in consultation with a TB expert."
Currently, people who have active TB are suggested to be treated using isolation techniques along with anti-TB drugs to prevent spread according to the CDC. The CDC suggests that patients with probable active TB be isolated in a private room with negative pressure (air exhausted to the outside or through a high-efficiency particulate air filter). Further, staff taking care of them must wear high-efficiency disposable masks sufficient to filter out any airborne mycobacteria. Continued isolation is suggested until sputum smears are negative for three consecutive determinations (usually after approximately two to four weeks of treatment). Sanatoriums (also spelled sanitorium or sanitarium) are where people with long-term illnesses, especially those with TB, used to be treated before good antibiotic therapy was available.
Researchers are attempting to produce an effective vaccine; there is a new study involving biobeads that contain several TB bacterial antigens and no live bacteria. The biobeads are being studied and may provide the first new vaccine against TB in 100 years.
Switzerland. World Health Organization. "Tuberculosis." Sept. 18, 2018. <http://www.who.int/mediacentre/factsheets/fs104/en/>.
United States. Centers for Disease Control and Prevention. "Tuberculosis (TB)." Oct. 22, 2018. <http://www.cdc.gov/tb/>.
Top Tuberculosis (TB) Facts Related Articles

Alcohol Abuse Slides
Read about the health risks of chronic heavy or binge drinking. Anemia, cancer, gout, cardiovascular disease and many more diseases can be caused by heavy or binge drinking.
C-Reactive Protein (CRP) Test
What are the ranges and levels of C-Reactive protein (CRP) in the blood? The CRP blood test is a marker of inflammation in the body, and it is produced by the liver. Find out about high, low, and normal ranges, levels, and results.
Chest Pain
Chest pain is a common complaint by a patient in the ER. Causes of chest pain include broken or bruised ribs, pleurisy, pneumothorax, shingles, pneumonia, pulmonary embolism, angina, heart attack, costochondritis, pericarditis, aorta or aortic dissection, and reflux esophagitis.
Diagnosis and treatment of chest pain depends upon the cause and clinical presentation of the patient's chest pain.

Chest X-Ray
Chest X-Ray is a type of X-Ray commonly used to detect abnormalities in the lungs. A chest X-ray can also detect some abnormalities in the heart, aorta, and the bones of the thoracic area. A chest X-ray can be used to define abnormalities of the lungs such as excessive fluid (fluid overload or pulmonary edema), fluid around the lung (pleural effusion), pneumonia, bronchitis, asthma, cysts, and cancers.
Is It Contagious Quiz
Is it contagious? Take this quiz to learn about contagious diseases, how contagious diseases are spread, and myths and facts about contagions.
Diabetes Mellitus (Type 1 and Type 2)
Diabetes is a chronic condition characterized by high levels of sugar (glucose) in the blood. The two types of diabetes are referred to as type 1 (insulin dependent) and type 2 (non-insulin dependent). Symptoms of diabetes include increased urine output, thirst, hunger, and fatigue.
What Are Lung Segmentectomy and Limited Pulmonary Resection?
A lung segmentectomy is a procedure to remove the diseased lung without removing excess normal lung. Lung segmentectomy and limited pulmonary resection are performed due to bonchiectasis, early-stage lung cancer, lung nodules, tuberculosis, and suppurative lesions. Complications include air leakage, bleeding, residual airspace, infection of the pleural space, respiratory failure, and cardiac complications.
Most Expensive Medical Conditions
What are the most expensive medical conditions? Learn about heart conditions, brain disorders, back pain and many more expensive health conditions. Discover the tips that can prevent serious medical problems and protect your financial well-being.
Night Sweats
Night sweats are severe hot flashes that occur at night and result in a drenching sweat. The causes of night sweats in most people are not serious, like menopause in women, sleep apnea, medications, alcohol withdrawal, and thyroid problems. However, more serious diseases like cancer and HIV also can cause night sweats. Your doctor will treat your night sweats depending upon the cause. You may experience other signs and symptoms that are associated with night sweats, which depend upon the cause, but may include, shaking, and chills with a fever caused by an infection like the flu or pneumonia; unexplained weight loss due to lymphoma; women in perimenopause or menopause may also have vaginal dryness, mood swings, and hot flashes during the day; and low blood sugar in people with diabetes. Other causes of night sweats include medications like NSAIDs (aspirin, acetaminophen, ibuprofen (Motrin, Advil), and naproxen (Aleve, Naprosyn), antidepressants, sildenafil (Viagra), and abuse of prescription or illegal drugs and drug withdrawal; hormone disorders like pheochromocytoma and carcinoid syndrome; idiopathic hyperhidrosis; infections like endocarditis, AIDs, and abscesses; alcoholism and alcohol withdrawal; drug abuse, addiction, and withdrawal; and stroke. A doctor or other health care professional can treat your night sweats after the cause has been diagnosed.
PCR (Polymerase Chain Reaction)
PCR (polymerase chain reaction) is a method to analyze a short sequence DNA or RNA. PCR (polymerase chain reaction) has many uses, for example, it is used to diagnose genetic diseases, establish paternity or biological relationships, DNA fingerprinting, DNA forensics, and finding bacteria and viruses.
Do I Have Pneumonia Quiz
Pneumonia can be deadly. Take the Pneumonia Quiz on MedicineNet to learn more about this highly contagious, infectious disease.
Swollen Lymph Nodes (Lymphadenopathy)
Lymph nodes help the body's immune system fight infections. Causes of swollen lymph nodes (glands) may include infection (viral, bacterial, fungal, parasites). Symptoms of swollen lymph nodes vary greatly, but may include fever, night sweats, toothache, sore throat, or weight loss. Causes of swollen lymph nodes also vary, but may include cancer, the common cold, mono, chickenox, HIV, and herpes. The treatment of swollen lymph nodes depends upon the cause.
Travel Health Slideshow
Explore travel health tips and vaccines to prevent disease while abroad. Learn to protect yourself against malaria, hepatitis, tetanus and more by learning which vaccines or health precautions are advised for your destination.
Tuberculosis PPD Skin Test
The tuberculosis skin test (also known as PPD, tuberculin, or Mantoux) determines whether a person has developed an immune response to the bacterium that causes tuberculosis (TB). Learn how doctors administer the TB test, obtain a reading, and interpret the results.
What Are the 3 Rarest Blood Types?
The red blood cells or RBCs present in the blood carry certain molecules, called antigens, on their surface that determine what blood group you have. The antigens depend on the genes you inherit from your parents. These antigens may be grouped in various categories to form a system for blood typing called the ABO system. The EldonCard blood type test kit uses the basic forward antibody technique of blood hematology for quick and simple determination of your blood type.