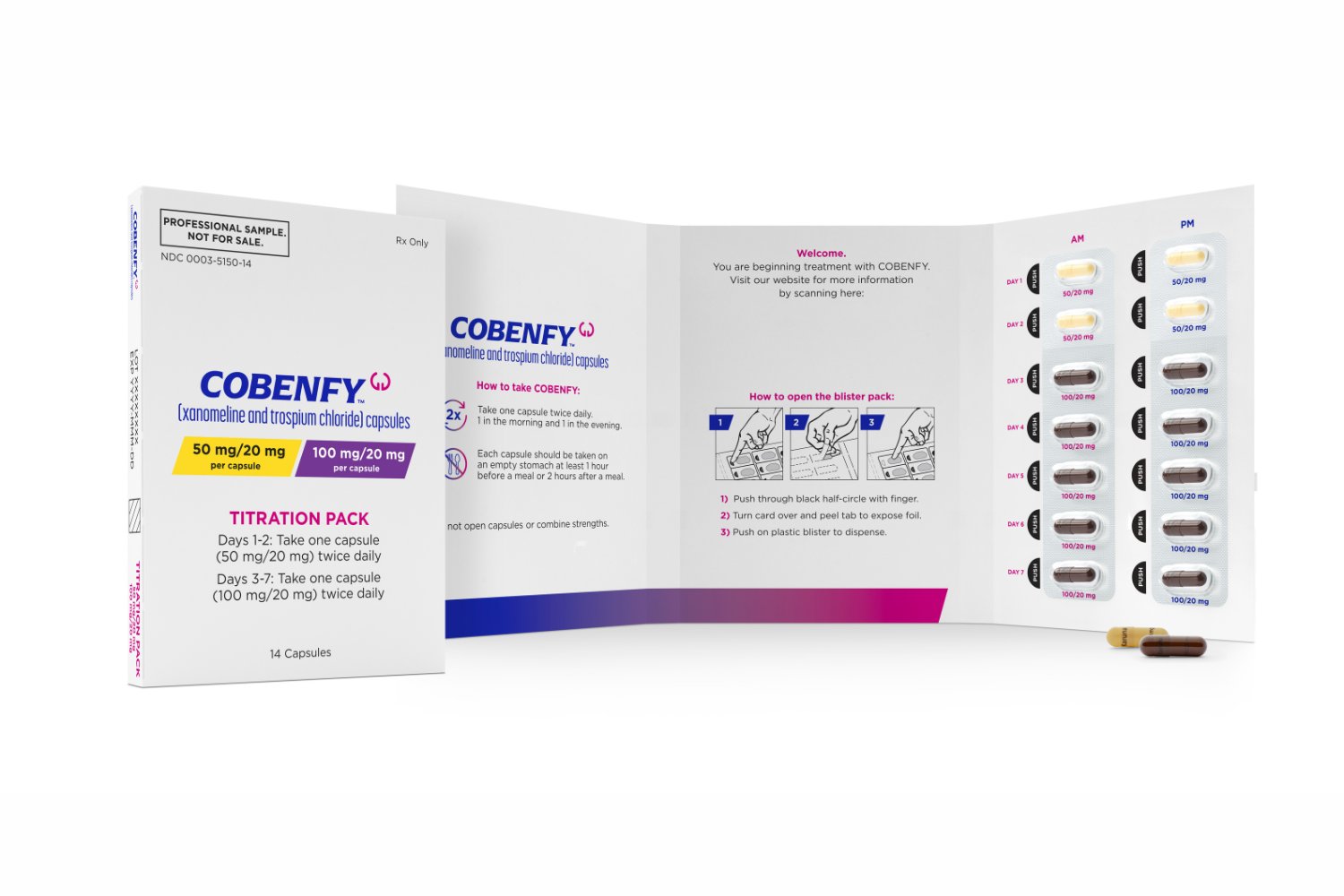
People living with schizophrenia will soon have a new and potentially groundbreaking treatment available. It’s called Cobenfy, and it’s the first new drug for the mental health condition to be successfully developed in over 70 years.
Cobenfy, now FDA-approved, is unique because it targets the neurotransmitter acetylcholine instead of focusing on dopamine, like traditional schizophrenia treatments. This could be a game-changer for patients who haven’t responded well to current meds or struggle with their side effects. With its approval, there’s new hope for better managing this challenging condition.
“This drug takes the first new approach to schizophrenia treatment in decades. This approval offers a new alternative to the antipsychotic medications people with schizophrenia have previously been prescribed,” said Tiffany Farchione, director of the Division of Psychiatry, Office of Neuroscience in the FDA’s Center for Drug Evaluation and Research, in the FDA’s announcement of its approval.
Schizophrenia is a severe psychiatric disorder, characterized by having intrusive thoughts, beliefs, and perceptions that are out of touch with reality. Less than one percent of the population has schizophrenia, which usually emerges in early adulthood, but it’s a devastating condition that can steadily destroy people’s lives, especially if not treated well. Current antipsychotic drugs and other interventions can reduce symptoms like hallucinations, but many people don’t respond to them or are unable to tolerate their harsh side-effects, such as weight gain or sexual dysfunction. So researchers have long been trying to find and develop new ways to treat schizophrenia that can overcome these limitations.
Over the years, scientists have created more tolerable antipsychotics, but these drugs have all worked on the same basic principle of targeting the production of the neurotransmitter dopamine in our brain (some schizophrenia symptoms, particularly hallucinations, are linked to too much dopamine in certain brain regions, while others are linked to too little dopamine elsewhere). Dopamine isn’t the only neurotransmitter involved in schizophrenia, though, and simply tweaking this one lever often isn’t enough to manage the illness. Cobenfy (formerly KarXT) is the first drug for schizophrenia to use a new mechanism of action since the 1950s, and the first to specifically target the neurotransmitter acetylcholine.
The drug (taken as a twice-daily pill) is actually two drugs in one: xanomeline and trospium chloride. Xanomeline stimulates two key receptors found on brain cells that interact with acetylcholine: muscarinic acetylcholine receptors 1 and 4 (M1 and M4). In past research, however, the drug alone has caused worrying adverse effects by activating these receptors outside of the brain, which originally led to its abandonment in clinical development. However, trospium chloride is a muscarinic receptor antagonist that doesn’t significantly cross the brain-blood barrier, ideally meaning that it can be used to counteract xanomeline’s off-target effects.
In the large-scale clinical trials reviewed by the FDA, Cobenfy appeared to work as intended. Compared to placebo, people on Cobenfy saw a significant improvement in their schizophrenia symptoms. The drug was also safely tolerated in general, though common side effects included nausea, indigestion, constipation, and vomiting. The drug will also not be recommended to people with a history of kidney or liver impairment, urinary retention, or certain forms of glaucoma.
Further research will be needed to confirm how well Cobenfy performs compared to other antipsychotics. But the simple virtue of being the first in a novel drug class can’t be overstated. The drug may be able to help people who haven’t responded to current therapies, and it’s likely to pave the way to other, possibly even more effective iterations that work in a similar fashion.
“Overall, I think this treatment does offer psychiatrists a completely new way of trying to help people with schizophrenia and I would expect that there will be some patients who will derive considerable benefit from it,” said David Curtis, a psychiatrist and honorary professor at University College London, in a response obtained by the Science Media Center in the UK.
As monumental as this drug is, however, it may not come cheap for many people. Bristol Meyer Squibbs has stated that the drug’s list price, before insurance and rebates, will be $1,850 for a month’s supply or $22,500 a year, though the company is set to start a program that will help support patients. It’s expected to hit the market by late October.